主题:Loeffler心内膜炎
心电图的T波低平一定是心肌缺血吗
嗜酸性粒细胞心内膜炎的临床及超声特点
患者 黄某某,43岁,
籍贯:四川 绵阳
无心血管疾病相关家族史
主诉:反复胸闷3月,伴发热1周
现病史:入院前3月患者无明显诱因出现胸闷,无胸痛心悸、无恶心呕吐,无发热盗汗,无黑曚晕厥,症状与运动无明显相关性。患者在当地医院就诊,行心电图检查等提示“心肌缺血”,给予“阿司匹林、丹参滴丸”等药物治疗。患者症状有所好转,但时有间断发作的情况发生。为求进一步治疗,患者到华西医院就诊,门诊行CT冠状动脉造影检查,结果提示冠状动脉粥样硬化斑块形成。考虑为“心脏神经官能症”,未予特殊处理。 入院前1周,患者开始间断性出现发热,最高体温38℃,无盗汗,无咳嗽咳痰,无咯血等不适。同时患者自觉胸痛症状有所加重。患者在当地医院经抗炎治疗后,发热症状已缓解,为求进一步治疗胸闷,患者遂再次到我院就诊。
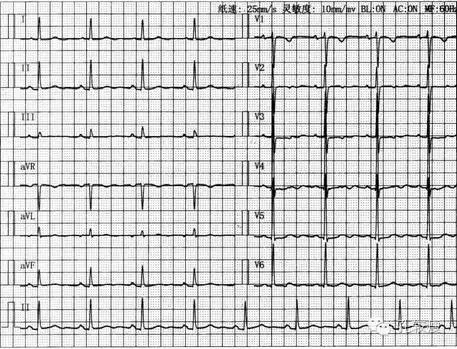
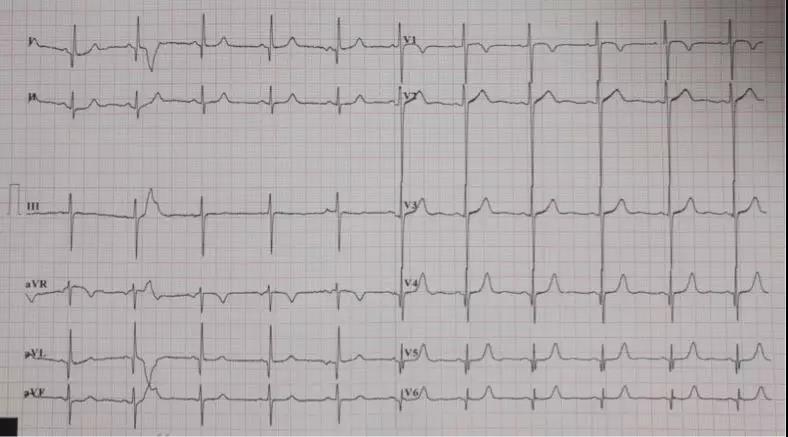
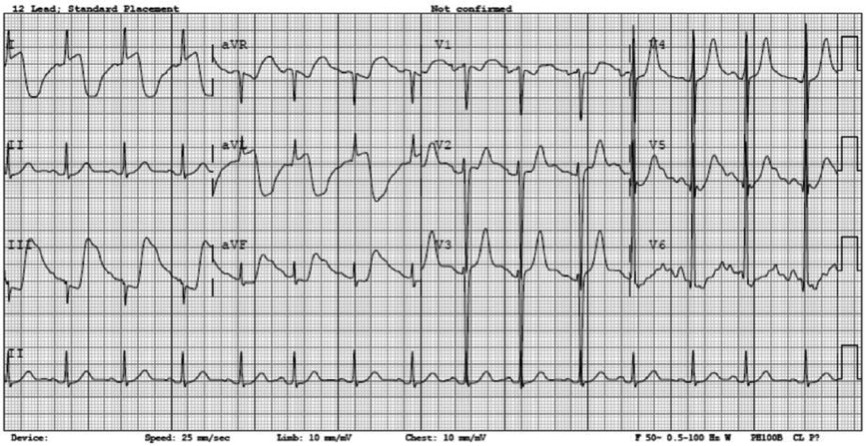
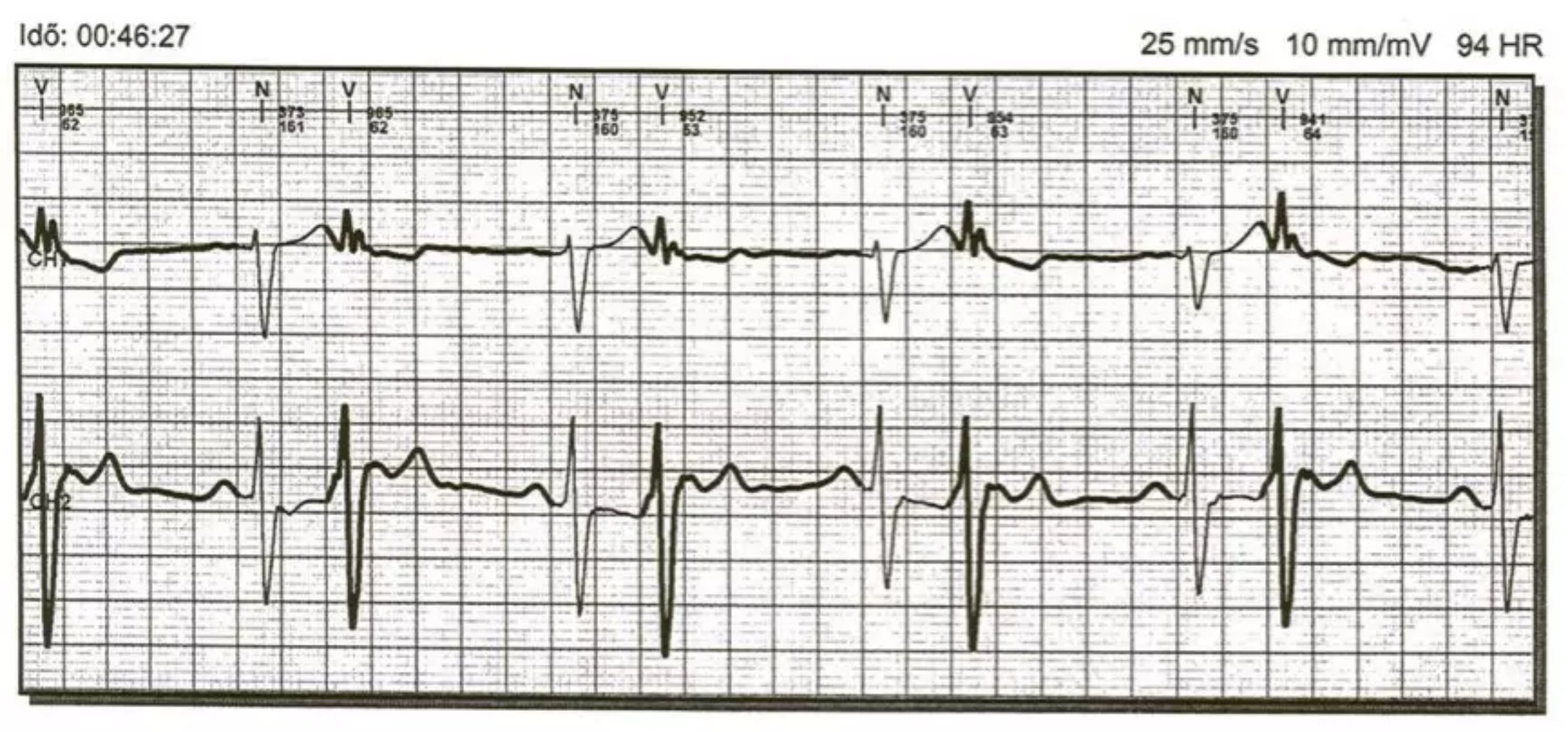
心电图检查提示广泛T波低平、部分导联T波倒置
体格检查提示生命体征平稳,二尖瓣听诊区可闻及2级收缩期吹风样杂音
当地医院CT检查提示左肺散在纤维条索影,左侧胸腔积液
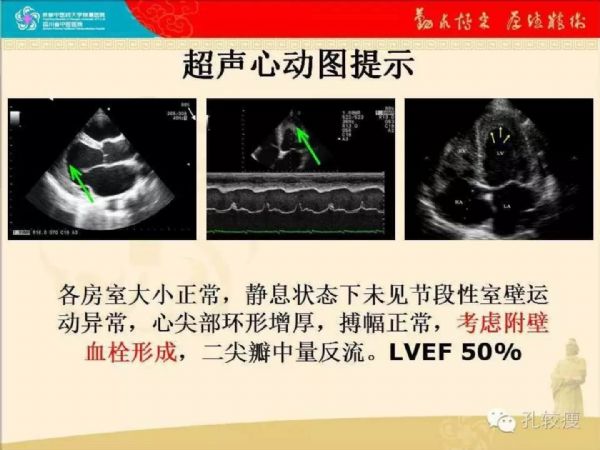
超声心动图检查提示左心室心尖处大量血栓形成(箭头)
心尖四腔心切面显示心尖处血栓形成,局部质地松软
组织多普勒显示心尖部运动状态尚可
左心室乳头肌短轴切面显示心内膜环形增厚
心尖处环形增厚,心尖接近闭塞
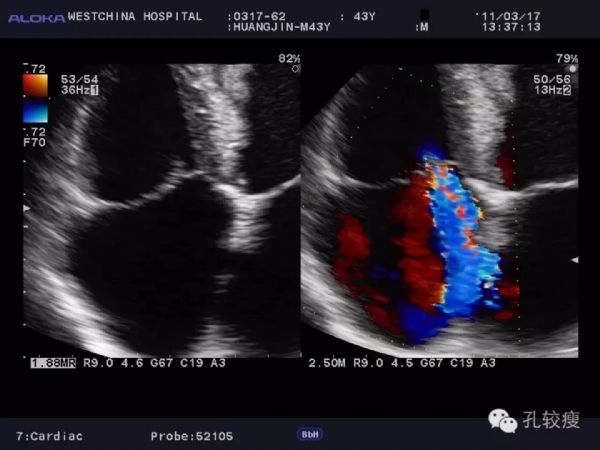
二尖瓣中量反流
三尖瓣中量反流
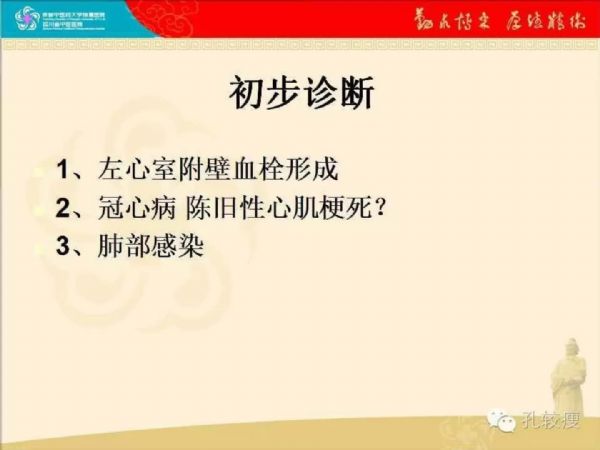
心电图检查提示广泛T波低平,既往冠脉CT检查未见确切冠状动脉狭窄及闭塞,但心脏超声检查发现左心室心尖处有附壁血栓形成。多数左心室内的血栓都是心肌梗死后室壁瘤血流瘀滞导致的,该患者下一步该如何考虑诊断及鉴别诊断?下一步的检查如何安排?
因为无法肯定是否冠状动脉是否有问题,所以决定还是复查冠状动脉造影检查,结果提示左右冠状动脉造影检查均未见明显异常
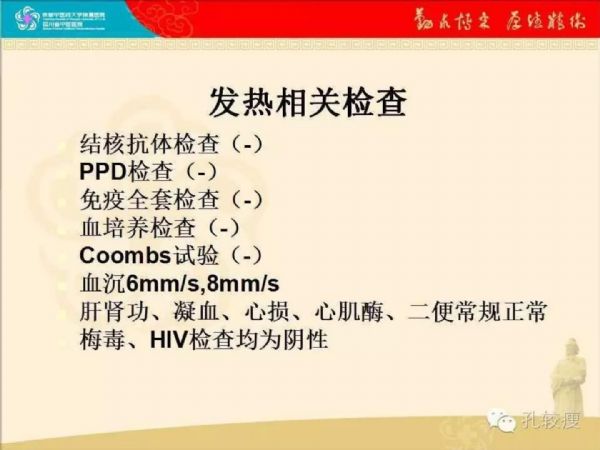
患者血常规检查结果提示嗜酸性粒细胞明显升高,追问病史患者无疫区居住史及接触史,不能除外特发性嗜酸性粒细胞增多症,遂给予强的松治疗,并且给予低分子肝素抗凝治疗
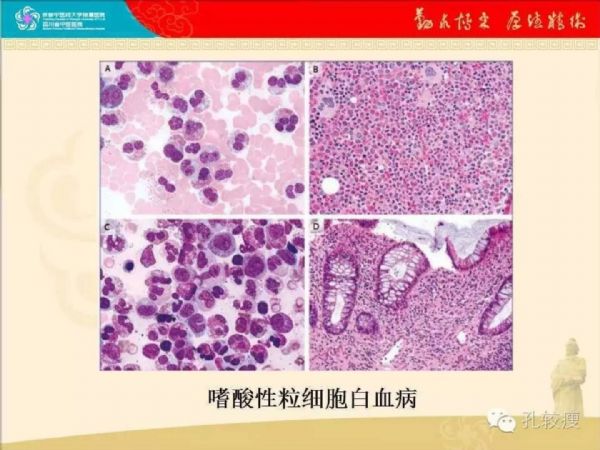
因药物治疗无效 ,行骨髓穿刺及活检提示嗜酸性粒细胞白血病
患者转血液科治疗,经羟基尿+HA等治疗后,病情无缓解;死于脑梗塞及感染
孔较瘦有话说
L?ffler心内膜炎血栓形成期超声表现,主要应与冠心病心肌梗死患者的左心室附壁血栓相互鉴别,后者系室壁运动降低后局部血流瘀滞所致,多伴有节段性室壁运动异常,冠状动脉造影可明确诊断。而L?ffler心内膜炎患者则局部心肌运动受限较轻,但随病程进展患者仍可出现室壁运动异常。需要注意的是,L?ffler心内膜炎的血栓形成机制及其主要成份不尽相同,但同样可出现心力衰竭及心源性衰竭等并发症。因此,临床除积极处理原发病外,还应加强抗栓治疗,以规避外周动脉栓塞。
本例患者在治疗中出现多发性脑梗塞,应与忽视抗栓方案有关。但因该病相对罕见,其抗栓方案是选择低分子肝素、华法林这类抗凝药物,抑或抗血小板聚集药物尚无定论,仍需病例积累及临床总结方能确定有效药物及其用法用量。
原始出处:
孔令秋,钟雪梅,王芳,唐红.嗜酸性粒细胞白血病致L(o)ffler心内膜炎及心原性栓塞一例[J].中华心血管病杂志,2015,43(11):1000-1001.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#腔内血栓#
37
谢谢分享学习了
77
#二尖瓣#
36
真是学到了知识.感谢老师
75