胸腔积液不简单 这个病因误诊率极高!
2018-07-11 冯起校 黄汉伟 专科医师培训指南---内科病例讨论
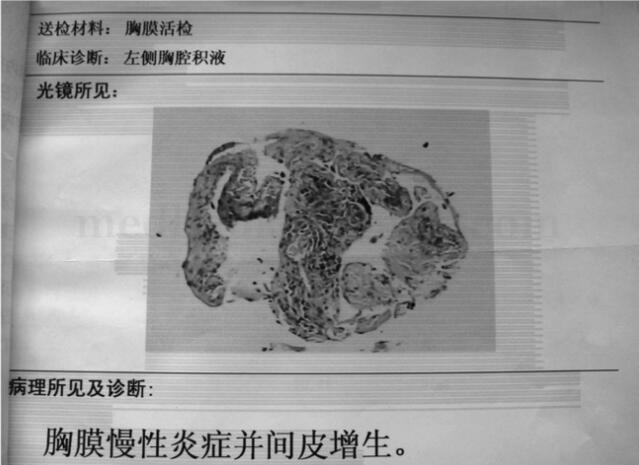
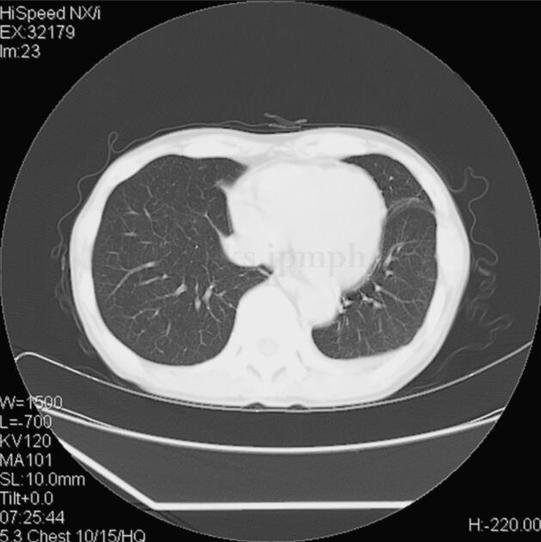
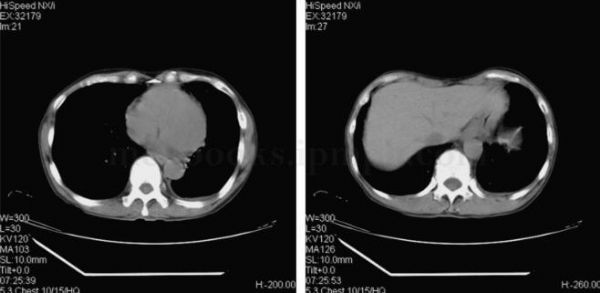
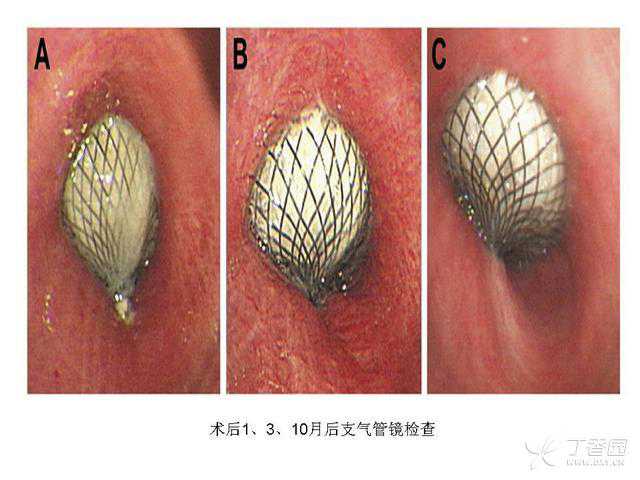
男性患者,64岁,因“左胸不适,左侧胸腔积液”第一次来院就诊,入院后经予左旋氧氟沙星、头孢曲松钠抗感染及对症支持等治疗,患者左胸不适症状缓解后出院。但出院后不久又出现左侧胸痛,呈间歇性隐痛,每次持续时间不等。7个月后,患者以“左侧胸痛半年余,伴胸闷、气促1个月余”为主诉再次入住治疗。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#误诊率#
43
学习
66
学习
72
学习
74
学习
84
学习
76
学习
18
学习
31
学习
30
学习
24