Science两篇:抗体疗法有望治愈HIV
2016-05-07 MedSci 生物谷
开发抗逆转录病毒疗法---延缓HIV体内复制的药物组合---已极大地改变了对HIV感染的治疗。曾经一度被宣判为死刑的HIV感染如今变成一种慢性疾病:病人能够携带HIV存活数十年。 但是这种疗法也有不足之处。它的副作用包括肾脏问题、骨密度下降和胃肠道问题。如果一个人停止他或她的治疗,甚至只是少服用几剂药物,人体内的HIV病毒水平就能够快速反弹。 来自美国洛克菲勒大学的研究人员与来自德国科隆大
开发抗逆转录病毒疗法---延缓HIV体内复制的药物组合---已极大地改变了对HIV感染的治疗。曾经一度被宣判为死刑的HIV感染如今变成一种慢性疾病:病人能够携带HIV存活数十年。
但是这种疗法也有不足之处。它的副作用包括肾脏问题、骨密度下降和胃肠道问题。如果一个人停止他或她的治疗,甚至只是少服用几剂药物,人体内的HIV病毒水平就能够快速反弹。
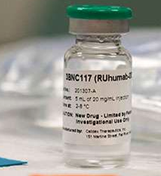
来自美国洛克菲勒大学的研究人员与来自德国科隆大学的研究人员合作,正在开发一种新的疗法:基于抗体的药物,它可能提供一种更好的用于长期控制HIV的策略。如今,根据一项I期临床试验开展的两项研究的结果,为抗体如何发挥功能提供新的认识。相关研究结果同时发表在2016年5月5日那期Science期刊上,论文标题分别为“HIV-1 therapy with monoclonal antibody 3BNC117 elicits host immune responses against HIV-1”和“Enhanced clearance of HIV-1–infected cells by broadly neutralizing antibodies against HIV-1 in vivo”。第一项研究是由来自洛克菲勒大学分子免疫学实验室的Michel Nussenzweig、Zanvil A. Cohn和Ralph M. Steinman领导的,其中Michel Nussenzweig教授是这项研究的通信作者,而这项研究的第一作者是来自洛克菲勒大学分子免疫学实验室的Till Schoofs、Florian Klein和Malte Braunschweig。第二项研究的通信作者是Michel C. Nussenzwei和来自洛克菲勒大学分子遗传学与免疫学实验室的Arup K. Chakraborty,第一作者是来自洛克菲勒大学分子免疫学实验室的Ching-Lan Lu。
Till Schoofs博士解释道,“这项研究提供证据证实单剂量抗体激活病人的免疫反应,使得这些病人能够制造针对HIV病毒的新的或更好的抗体。”
Schoofs博士补充道 ,“我们去年已报道这种治疗能够极大地降低病人血液中存在的HIV病毒数量,但是我们想要在更长时间内追踪这些病人以便研究他们的免疫系统如何适应这种新疗法。”
中和一种致命的病毒
这项研究中使用的一种被称作3BNC117的广泛中和抗体分子能够抵抗很多HIV毒株。作为Nussenzweig实验室的一名学生,Johannes Scheid在几年前分离出这种抗体,而且是从一名HIV感染者---这名感染者的免疫系统通过阻止HIV感染和破坏一种特定的被称作CD4 T细胞的免疫细胞而能够很好地中和血液中的HIV---体内分离到的。CD4 T细胞遭受破坏是AIDS(获得性免疫缺陷综合征,俗称艾滋病)产生的一种典型特征。
早前的研究已证实3BNC117能够中和在全世界发现的80%以上的HIV毒株。因此,研究人员猜测将这种抗体注射进病人体内也将有助他们抵抗HIV病毒,为此开展一项临床试验。
这项临床试验涉及15名血液中具有高水平HIV的病人,和12名已接受抗逆转录病毒疗法(ART)治疗而使得病毒水平得到控制的病人。这项临床试验的参与者绝大多数是在洛克菲勒大学医院接受治疗。将单剂量3BNC117抗体注入到这些病人体内,在一个月内对他们进行监控。
研究人员发现在这15名血液中具有高水平HIV的病人当中,14人在接受这种抗体注射后能够制造新的抗体,而且这些新的抗体能够中和一些不同的HIV毒株。
Schoofs说,“人体通常需要好几年时间才开始制造好的抗HIV抗体。因此,随后可能产生更好的效果,特别是如果病人接受不止一剂3BNC117注射。”
这项研究的下一步就是测试3BNC117与其他靶向作用于HIV的抗体的组合使用,以便确定是否观察到一种更加强大的抗病毒效果。研究人员也正在开展II期临床试验,在这项临床试验中,接受ART治疗的病人转向接受抗体治疗。
探究抗体功能
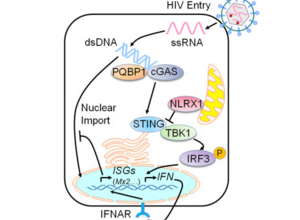
在第二项研究中,研究人员想要确定3BNC117抗体治疗是否可能具有比ART治疗更多的益处。
他们研究了第一项临床试验的研究结果,然后采用一种HIV动力学数学模型来预测如果3BNC117只是中和血液中的HIV和阻断新的HIV感染产生,那么这些病人体内的HIV水平如何变化。他们的分析证实中和HIV单独并不能解释在病人体内观察到的病毒水平急剧下降,这就让他们猜测肯定存在另一种组分增强这种抗体的疗效。
通过针对模式小鼠开展研究,研究人员提供证据证实3BNC117能够调动小鼠体内的免疫细胞,加快它们清除被HIV感染的细胞。Ching-Lan Lu说,“这证实这种抗体不仅能够对HIV病毒施加压力,而且也能够缩短被感染细胞的存活时间。我们的结果解释了在我们的模式小鼠体内,为何基于抗体的暴露后预防(post-exposure prophylaxis,也译作接触后预防)”---暴露后预防指的是在接触HIV后接受短期治疗降低感染---“要比ART治疗更加有效。”
此外,研究人员可能潜在地解决了治愈HIV感染的一个主要障碍:HIV在感染后不久能够在人体内建立潜伏的病毒库,从而潜藏在人体内,逃避治疗。一项追踪临床研究正在洛克菲勒大学开展,以便评估接受ART治疗的病人接受抗体药物注射后是否能够有助降低或改变这些病人的HIV病毒库。
原始出处:
HIV-1 therapy with monoclonal antibody 3BNC117 elicits host immune responses against HIV-1.Science.doi:10.1126/science.aaf0972
Enhanced clearance of HIV-1–infected cells by broadly neutralizing antibodies against HIV-1 in vivo.Science.doi:10.1126/science.aaf1279
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#SCIE#
37
#抗体疗法#
50
学习了,很好的
125
真的不错!
49
这是真的吗
122
不会是莆田吧
100