Lancet Oncol:突破!科学家首次证实,基于CT影像的人工智能算法可以判断癌症患者能否从免疫治疗中获益
2018-09-04 奇点糕 奇点网
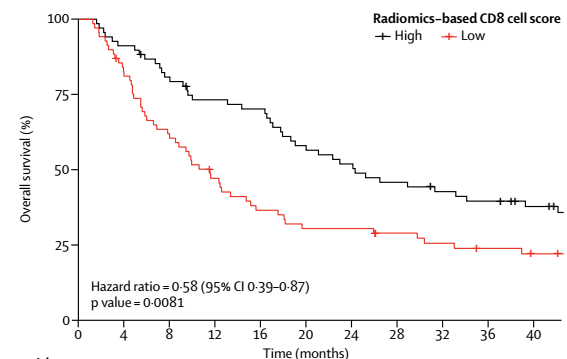
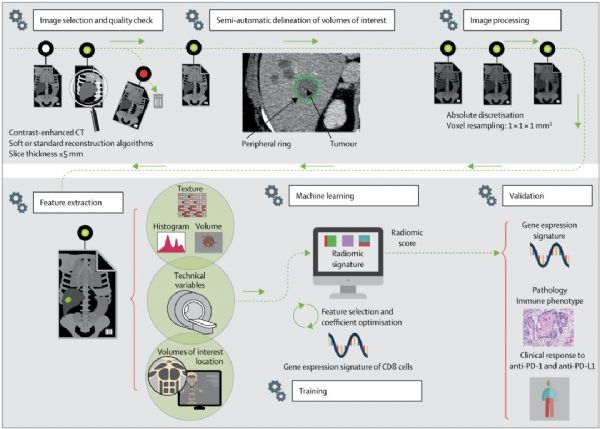
近日,来自法国的Eric Deutsch博士团队借助人工智能之力,给我们带来了新的希望。他们用癌症患者的CT图像训练人工智能,得到一个可以通过患者的CT影像准确预测PD-1抑制剂治疗效果的人工智能平台。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Lancet#
48
#首次证实#
44
#Oncol#
37
学习
94
#癌症患者#
43
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
74
学习谢谢分享
72
学习了
81
学习了,谢谢分享
86
学习了,谢谢作者分享!
21