我的设计我做主:MedSci临床研究方案设计活动-立题公布(2)
2015-05-13 MedSci MedSci原创
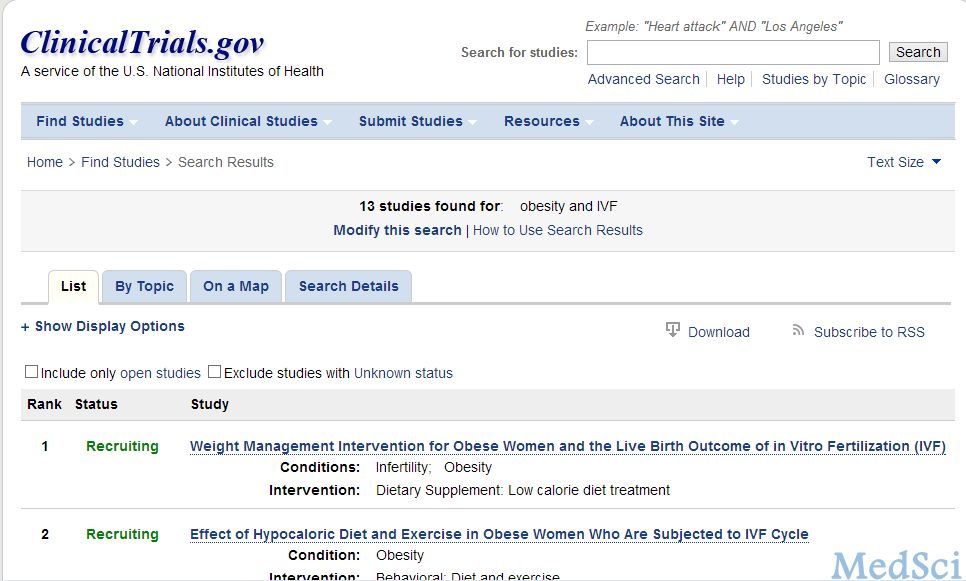
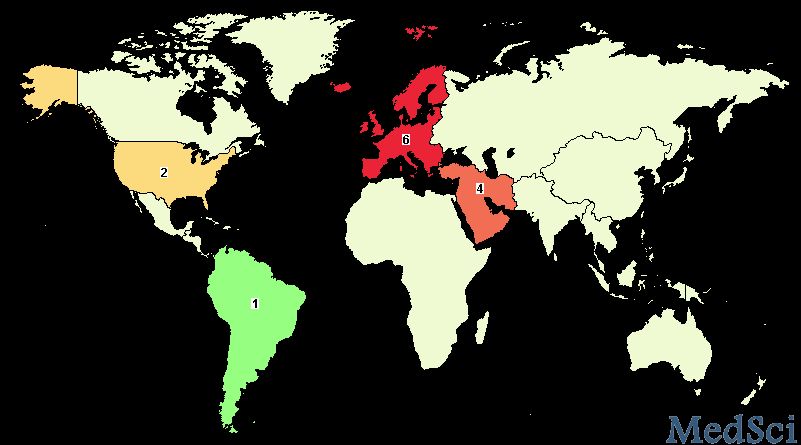
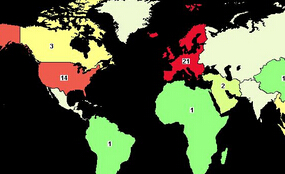
前提示:【我的设计我做主】MedSci临床研究方案设计活动-立题公布(1)对于肥胖或体重超标者实施体重控制或干预(减轻体重)对于IVF妊娠结局的影响对于肥胖或体重超标者实施体重控制或干预(减轻体重)对于IVF妊娠结局的影响 相关的研究成果不少(fig 1 Pubmed上粗略的检索结果),正在进行或已经结束的注册研究也有一些(fig 2 www.clinicaltrials.gov上注册的研究,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#方案设计#
33
#研究方案#
49
认真学习
50
看看
119
#Med#
30
看看
59