腹腔镜胰腺切除术中并发甲亢一例
2020-08-07 许巧巧,代金贞 临床外科杂志
病人,女,50岁,身高157 cm,体质量40kg。因间断上腹痛1年余,加重5天就诊。腹部CT检查提示胰头、体交界部囊性占位。有明显消瘦、血糖增高病史,余无特殊。血、尿常规、肝肾功能无异常,血糖7.0
病人,女,50岁,身高157 cm,体质量40kg。因间断上腹痛1年余,加重5天就诊。腹部CT检查提示胰头、体交界部囊性占位。有明显消瘦、血糖增高病史,余无特殊。血、尿常规、肝肾功能无异常,血糖7.05mmol/L。
心电图检查窦性心律,心率89次/分钟。心脏彩超:EF62%,E峰92 cm/s,A峰86 cm/s。胸部X线片检查无异常。磁共振—胆道成像检查提示胰腺体部囊性占位,肿瘤性病变可能。临床诊断为胰腺肿物。在全麻下行腹腔镜下胰体尾病损切除术。
选择静注咪唑安定0.5mg,依托咪酯14mg、罗库溴铵40mg、芬太尼0.15mg快速诱导,经口腔明视下气管内插管。以静脉持续泵注瑞芬太尼、丙泊酚,复合低浓度七氟烷吸入,间断静注肌松剂阿曲库铵维持麻醉,机械通气。
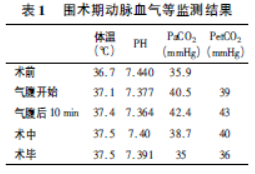
围术期常规监测心电图、体温、氧饱和度、呼气末二氧化碳、有创及无创动脉血压、间断监测血气。手术开始,有创动脉血压125/66mmHg、心率93次/分钟、咽温36.6℃、呼气末二氧化碳39mmHg。二氧化碳气腹建立后10分钟,血压139/74mmHg。心电图检查心率97次/分钟进行性增快至120次/分钟左右、体温进行性上升至37.5℃并持续,呼气末二氧化碳增高至43mmHg。血气分析显示:未见高碳酸血症(表1)。
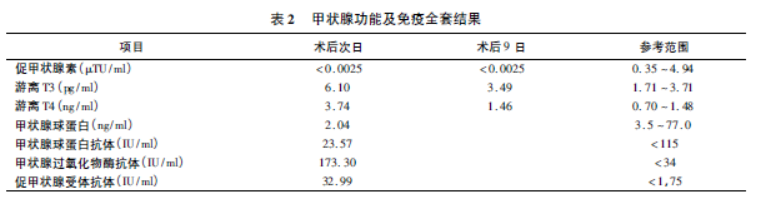
经冰盐水持续输注及静注地塞米松、双侧颈动脉体表酒精擦拭,调整静吸复合麻醉:减低七氟烷吸入浓度,增加静脉麻醉药丙泊酚、瑞芬太尼泵注剂量及间断静注芬太尼,应用β受体阻滞剂艾司洛尔控制心率,至二氧化碳气腹结束时,血压147/82mmHg,心率仍维持于120~130次/分钟,咽温37.5℃~37.4℃。术毕,血压129/81mmHg、心率130次/分钟,病人意识恢复,气管插管拔除后转入麻醉恢复室。术后急查甲状腺功能及免疫全套提示甲状腺功能亢进,疑为导致术中心率增快、体温增高原因。对症给予赛治每日口服10mg治疗,甲亢体征逐步控制:体温自37.5℃降至37.0℃、血压120/80mmHg降至110/70mmHg、脉搏100次/分钟降至63次/分钟。术后10天复查甲状腺功能,明显改善(表2)。
讨论
腹腔镜手术具有创伤小、恢复快、术后疼痛轻、住院时间短等,广泛应用于外科、妇产科等领域。人工气腹是腹腔镜手术的必要条件,目前临床上普遍采用二氧化碳人工气腹,可引起高碳酸血症、腹内压和胸内压增加、对循环产生影响、二氧化碳气栓、二氧化碳排除综合征等并发症。
警惕腹腔镜手术并发症是围术期关注的重点。本例术前既往病史中未提示有甲状腺方面疾病,甲状腺功能未作为术前常规检查。另外,病人常规心电图及入手术室后的生命体征均未提示存在甲亢征象。病人在腹腔镜胆囊切除手术人工气腹开始10分钟后随即发生心率进行性增快,体温进行性增高,但并未出现呼气末二氧化碳持续增高,可首先排除凶险并发症恶性高热(malignant hyperthermia,MH)。
MH的发生多与挥发性吸入麻醉药和肌松剂琥珀酰胆碱所触发的骨骼肌异常高代谢状态有关,以先天性疾病如持发性脊柱侧弯、斜视、上睑下垂、脐疝、腹股沟疝等多见。恶性高热常表现为高碳酸血症和高钾血症、快速心律失常、酸中毒、体温急剧升高等。本例血气分析可证实和排除恶性高热。因此,腹腔镜手术中的体温、血气监测尤为重要,不可忽视。
有研究表明,腹腔镜手术对应激反应的影响小于开腹手术,因此,手术及麻醉本身对应激水平的影响不会直接导致本例急进性心动过速及发热,在二氧化碳气腹的干扰因素撤除后心率仍居高不下,可排除二氧化碳气腹对应激水平的影响。在进一步对症给予双侧颈动脉体表酒精擦拭及冰生理盐水输注等降温措施,追加镇痛药物及β受体阻滞剂控制心率处理后,效果仍不明显。经术中急查甲状腺功能及免疫全套,确诊为腹腔镜术中并发甲亢。
非甲状腺手术腹腔镜手术术中诱发甲亢,鲜有发生,本例即为腹腔镜手术中并发甲亢的典型案例。麻醉和手术是常见的促发因素。本案例提示,在有条件的医疗单位,腹腔镜手术病人术前甲状腺功能的检测对围术期管理有帮助。
原始出处:
许巧巧,代金贞.腹腔镜胰腺切除术中并发甲亢一例[J].临床外科杂志,2019,27(08):692-693.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#并发#
27
#切除术#
28
#胰腺切除#
44
#胰腺切除术#
30
#腹腔镜#
30
棒
96