手法复位罕见肩关节脱位1例
2019-08-21 方成 甘泉 江昭林 实用骨科杂志
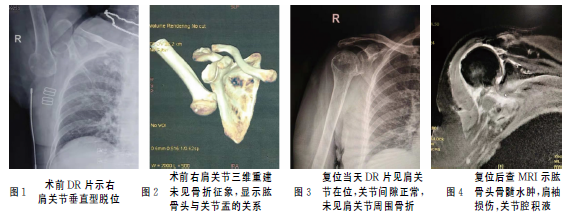
患者,女,68岁,因“车祸致右肩关节疼痛、活动受限0.5h”入院。体格检查:神志清楚,表情痛苦,右上臂上举、屈肘,方肩畸形,右肩关节弹性固定,关节盂空虚,腋窝下方可触及脱出的肱骨头,肩关节压痛(+)。右肩关节DR片提示右侧肱骨头完全脱出于关节盂下方,肱骨头朝下,肱骨干与躯干呈135°夹角(见图1);进一步行右肩关节CT及三维重建未见骨折征象(见图2)。入院诊断:右肩关节脱位———垂直型脱位。采用手
临床资料
患者,女,68岁,因“车祸致右肩关节疼痛、活动受限0.5h”入院。体格检查:神志清楚,表情痛苦,右上臂上举、屈肘,方肩畸形,右肩关节弹性固定,关节盂空虚,腋窝下方可触及脱出的肱骨头,肩关节压痛(+)。右肩关节DR片提示右侧肱骨头完全脱出于关节盂下方,肱骨头朝下,肱骨干与躯干呈135°夹角(见图1);进一步行右肩关节CT及三维重建未见骨折征象(见图2)。入院诊断:右肩关节脱位———垂直型脱位。采用手法复位:首先5mL盐酸利多卡因与生理盐水1︰1稀释,关节腔及三角肌周围浸润麻醉,待患者疼痛症状好转,术者沿上臂畸形方向外上方牵引患肢,助手自腋窝下方向关节盂方向推挤肱骨头,术者一边牵引一边内收上臂复位。成功复位后肩关节被动活动正常,关节盂饱满,方肩畸形消失,Dugas征(-),复查DR右肩关平片见肩关节在位,关节间隙正常,未见肩关节周围骨折征象(见图3)。嘱患者右肩部三角巾悬吊制动3周。进一步行右肩关节MRI检查了解肩袖损伤情况(见图4)。复位后患者右肩部感觉无麻木,右肘关节、前臂及手指活动,感觉正常,提示复位过程中无腋神经及臂丛神经损伤。3个月后门诊复查见右肩关节功能良好。
讨论
肩关节是由肱骨头及肩胛骨的关节盂组成的球窝关节,关节盂小而浅,关节囊薄而松弛,是活动范围最广的关节,可以主动做外展、内收、前屈、后伸、外展、旋转及环转运动。这些解剖学特点也决定了肩关节是最容易脱位的关节(其次多见于肘关节),肩关节脱位发生率占全身关节脱位的50%,是肘关节脱位发生率的3倍。肩关节脱位在临床上以前脱位最常见,约占95%,后脱位相对少见,占1.8%~4.3%。垂直型脱位是肩关节脱位一种罕见脱位类型,该类型特点是肱骨头完全脱出后交锁于关节盂窝下方,上臂上举,无法内收运动。
查找国内外相关文献关于此类肩关节脱位详细报道较少。该类型脱位虽属罕见,但往往肩关节周围软组织损伤严重,其原因是由于其特殊受伤机制导致。垂直型脱位发生于上臂极度外展,外力作用上臂,上臂以肱骨头为旋转轴,以肩峰为杠杆,将股骨头撬出关节囊至关节盂下方。复位后查肩关节MRI同样证实,这种极度外展及旋转暴力导致严重的关节囊周围软组织及韧带损伤。就肩关节脱位复位经验而言,我们在关节腔及关节周围多个方向浸润注射麻醉药,均成功手法复位,避免采用静脉麻醉或神经阻滞麻醉,繁琐的术前准备,不仅增加患者医疗费用,而且可能造成一些神经损伤。复位前尽量完善肩关节CT,尤其老年患者,排除一些隐匿性骨折线存在。本例患者同样采用局部浸润麻醉成功手法复位,无血管及神经损伤,临床效果满意。
原始出处:
方成,甘泉,江昭林,王鹏浩,赵文.手法复位罕见肩关节脱位1例报道[J].实用骨科杂志,2019,25(07):668-669.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#关节脱位#
35
#肩关节#
50
#罕见#
24
#脱位#
33