SCRT:胎盘间充质干细胞治疗缺血性疾病又有新发现
2016-05-28 赵广立 中国科学报
近日,国家干细胞工程技术研究中心主任韩忠朝团队发表在Stem Cell Research & Therapy上的一篇题为《VCAM-1+胎盘绒毛膜间充质干细胞显示出强有力促血管生成活性》的文章受到国内外相关领域的高度关注。该文章阐述了血管细胞黏附分子-1+(VCAM-1+)胎盘绒毛膜间充质干细胞(CV-MSC)具有良好的促血管生成活性,成为理论走向临床治疗的重要一步。 许多研究已经证
近日,国家干细胞工程技术研究中心主任韩忠朝团队发表在Stem Cell Research & Therapy上的一篇题为《VCAM-1+胎盘绒毛膜间充质干细胞显示出强有力促血管生成活性》的文章受到国内外相关领域的高度关注。该文章阐述了血管细胞黏附分子-1+(VCAM-1+)胎盘绒毛膜间充质干细胞(CV-MSC)具有良好的促血管生成活性,成为理论走向临床治疗的重要一步。
许多研究已经证明,来自不同组织源的间充质干细胞对缺血性疾病有不同程度的治疗效果,有研究人员认为是由于间充质干细胞的旁分泌作用,然而机制尚不明确。
该研究分离了胎盘绒毛膜来源的VCAM-1+间充质干细胞亚群,在血管生成的不同阶段以及不同水平上研究了VCAM-1+间充质干细胞和VCAM-1-间充质干细胞的性质,评估了其促血管生成能力,探讨了其在缺血性疾病上的应用价值。
该研究显示,8个血管生成基因(HGF、ANG、IL8、IL6、VEGF-A、TGFβ、MMP2和bFGF)高表达于VCAM-1+胎盘绒毛膜间充质干细胞;同样,血管生成细胞因子特别是HGF、IL8、angiogenin、angiopoitin-2、μPAR、CXCL1、IL-1β、IL-1α、CSF2、CSF3、MCP-3、CTACK和OPG在VCAM-1+胎盘绒毛膜间充质干细胞中显著增加。将VCAM-1+胎盘绒毛膜间充质干细胞输注到BALB/c裸鼠的缺血后肢,其下肢功能显著改善,证明了VCAM-1+胎盘绒毛膜间充质干细胞具有良好的旁分泌促血管生成效果,可作为相关疾病的重要治疗手段。
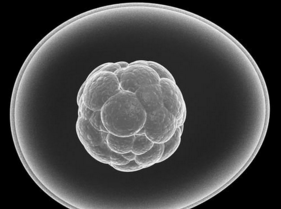
VCAM-1又被称为CD106,属于免疫球蛋白超家族,是重要的黏附分子,被认为在动脉粥样硬化和类风湿性关节炎的发病过程中具有重要的作用。VCAM-1在早期胚胎发育中也起着至关重要的作用,胚胎早期缺乏VCAM-1会导致胎盘严重缺陷。
韩忠朝团队长期关注胎盘绒毛膜来源的VCAM-1+间充质干细胞(VCAM-1+CV-MSC)。此前,该团队就已经通过大量实验认识到VCAM-1+CV-MSC分泌前列腺素E2的能力很强,能强烈抑制植物血凝素(PHA)刺激的人外周血单个核和脐血CD4+T细胞的IFN-γ和TNF-α的分泌,并能有效地降低CD4+T细胞内IFN-γ、TNF-α、T-bet、IL-21和IL-22的表达。基因芯片结果也显示VCAM-1+CV-MSC表达更多的免疫相关基因,证实了VCAM-1+CV-MSC是一个具有很强免疫调节功能的亚群。
目前已有大量国内外研究表明VCAM-1可能参与血管生成。一般情况下,VCAM-1在静息的内皮细胞低表达或不表达,但可以被各种炎症因子诱导表达,如VCAM-1可在活化的血管内皮细胞中表达;CV-MSC可以组成性地表达VCAM-1,除了膜结合的形式,还有可溶性的VCAM-1存在。
因此,VCAM-1可以作为表面标记物来进行间充质干细胞优越亚群的筛选,为将来间充质干细胞在临床上应用于治疗心肌梗死、中风等缺血性疾病提供了新的策略,也为将来临床治疗上提供了一种高效的间充质干细胞亚群。
我国正逐步进入老龄化社会,严重肢体缺血的外周动脉疾病呈多发病率趋势,死亡率也逐年上升。目前的主要手术治疗手段效果并不理想。因此,间充质干细胞的这种促血管生成特性受到临床上的高度关注。
干细胞生物技术是当今生命科学领域前沿技术,在疾病预防、治疗和抗衰老、美容等方面有着广泛的应用前景。在我国,干细胞技术先后被列入“863”“973”等重大科研专项。其中,胎盘来源的间充质干细胞具有免疫原性低、活力较强、无伦理问题等优点,成为近几年研究的焦点。
原始出处:
Du W, Li X, Chi Y, Ma F, Li Z, Yang S, Song B, Cui J, Ma T, Li J, Tian J, Yang Z, Feng X, Chen F, Lu S, Liang L, Han ZB, Han ZC. VCAM-1+ placenta chorionic villi-derived mesenchymal stem cells display potent pro-angiogenic activity. Stem Cell Res Ther. 2016 Apr 4;7:49. doi: 10.1186/s13287-016-0297-0.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#新发现#
22
#缺血性#
18
#间充质干细#
29
#CRT#
0
#胎盘#
22
#SCR#
0