Aliment Pharmacol Ther:走向克罗恩氏病和类风湿关节炎的共同治疗目标
2017-05-13 应颖秋;常路 环球医学
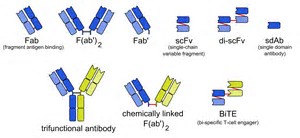
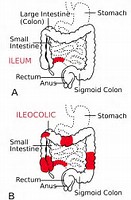
克罗恩氏病(CD)和类风湿关节炎是慢性的进展性和致残性疾病,常可造成结构组织损伤。基于原先开发的类风湿关节炎的策略,最近,CD的治疗目标已经从完全控制症状转移到临床缓解和完全黏膜愈合(深度缓解),最终的目的为防止肠道损伤和残疾。2017年4月,发表在《Aliment Pharmacol Ther》的一项综述回顾CD和类风湿关节炎治疗目的的相似性和差异。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Pharm#
34
#克罗恩氏病#
38
#pharma#
33
#Pharmacol#
20
#MAC#
0
学习了,长见识了
67
学习了,感谢分享!
64
学习了,多谢分享
61
学习了,谢谢
56
学习一下知识
57