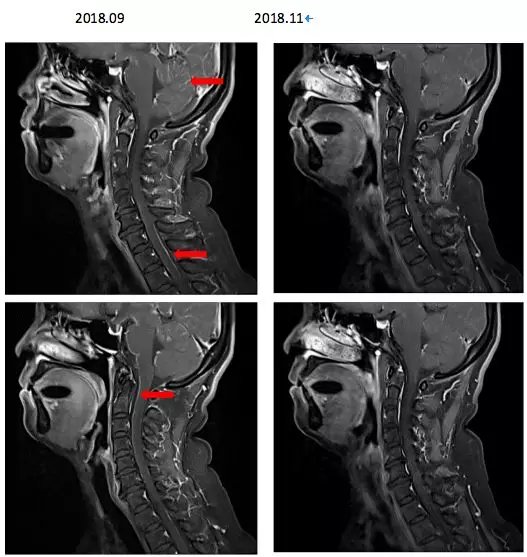
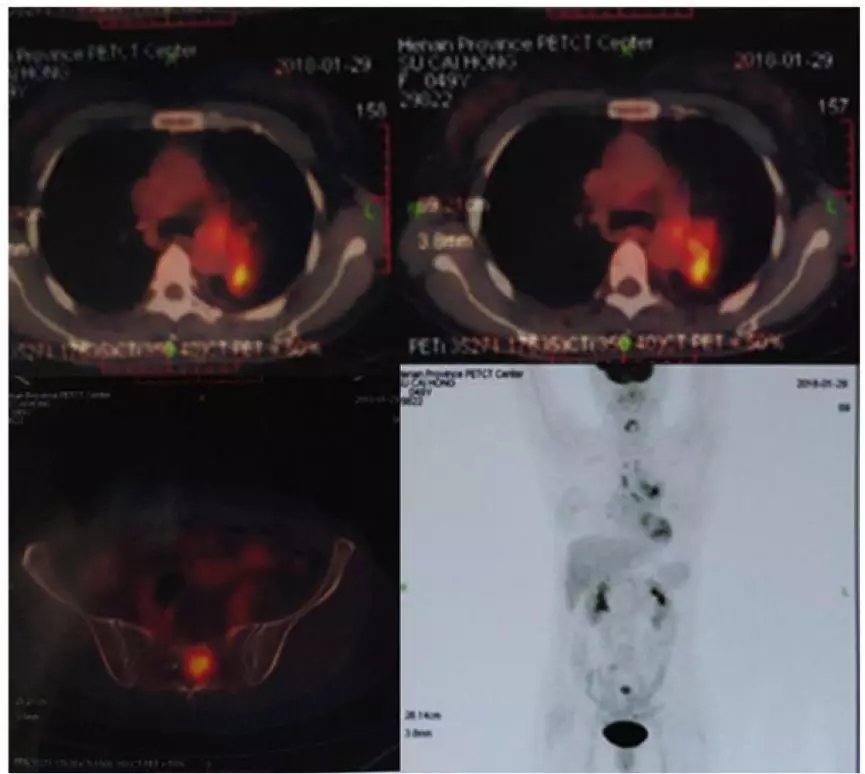
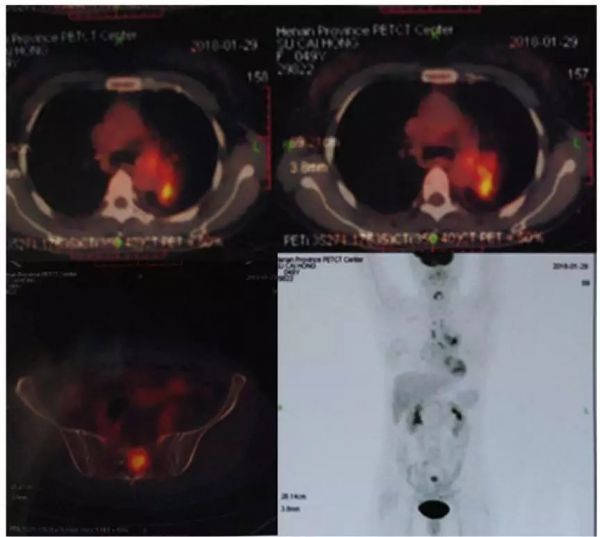
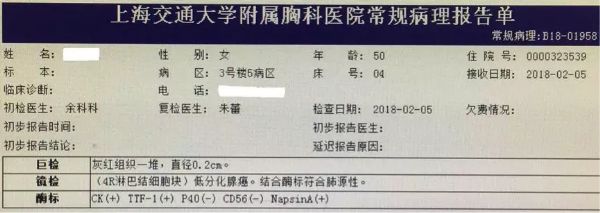
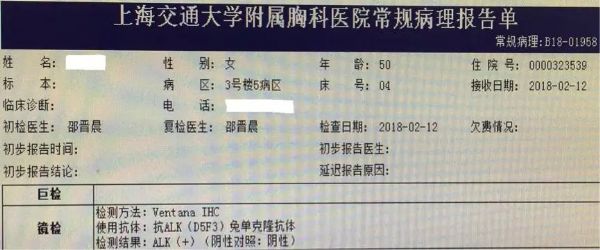
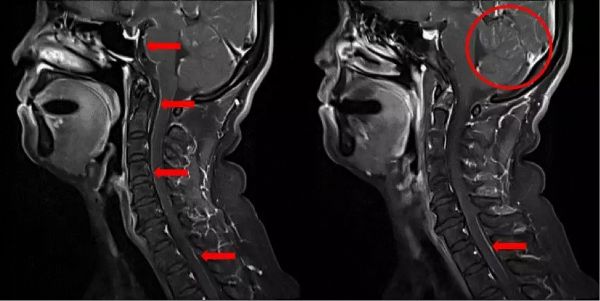
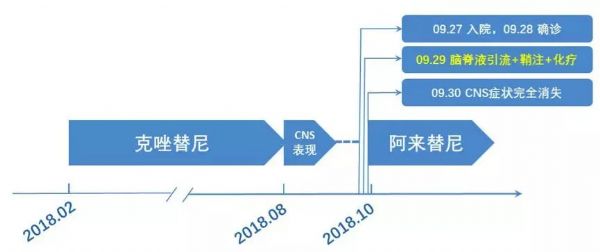
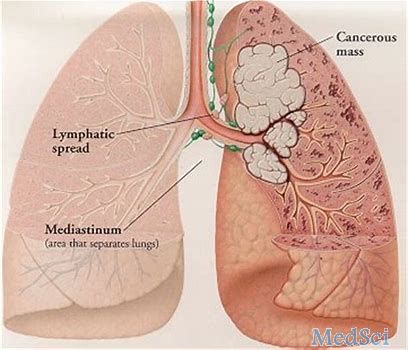
ALK+脑膜转移晚期肺腺癌患者诊疗带来的总结与思考
2018-12-30 李醒亚 肿瘤资讯
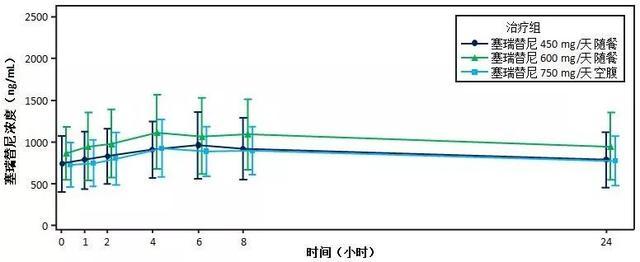
脑膜转移(leptomeningeal metastasis,LM)是晚期非小细胞肺癌(non-small cell lung cancer,NSCLC)严重并发症之一,发病率低,预后差。NSCLC患者在治疗过程中约40%~55%的患者会出现脑转移,脑转移患者中约10%为脑膜转移,合并基因突变患者靶向治疗后脑/脑膜转移发生率升高。由于起病隐匿,临床表现缺乏特异性,脑膜转移早期诊断困难。因此,临床上

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ALK+#
46
#晚期肺腺癌#
47
学习
86
学习
79
学习
83
学习
66
学习
75
学习
30
学习
0
学习
0