Ultrasound:超声检查或可提高血管疾病早期检出率
2018-09-01 佚名 嘉音
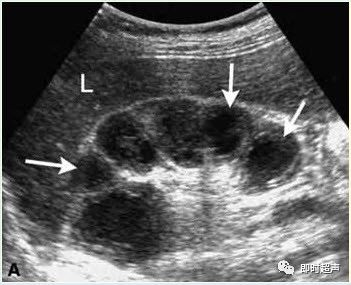
8月7日,在线发表于《Ultrasound》杂志上的一项研究表明,在血管疾病患者表现出症状前,血管超声就可以提高其早期检出率。动脉粥样硬化和腹主动脉瘤是常见的血管疾病,该疾病平时较为隐匿,但发病时往往危及生命,早期诊断对不良事件的预防至关重要。采用血管超声对动脉血管壁的生物力学指标进行检测,如动脉随心脏收缩和舒张的搏动能力,有可能成为诊断血管疾病的早期指标。莱斯特大学生命科学学院领导的研究团队与莱
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Ultra#
34
#Sound#
40
#TRA#
29
#ultrasound#
45
#检出率#
39
#ASO#
36
#超声检查#
37
#血管疾病#
27
超声可提高血管疾病早期检出率。
72
有用
66