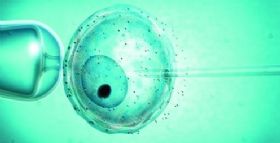
JAMA Pediatr:试管婴儿的孩子出生缺陷更高?
2016-04-08 MedSci MedSci原创
一项美国的研究报道指出,体外受精 (IVF) 或使用其它生殖技术的女性相比自然受孕的更容易发生后代出生缺陷。
一项美国的研究报道指出,体外受精 (IVF) 或使用其它生殖技术的女性相比自然受孕的更容易发生后代出生缺陷。
作者注意到这项发现将女性尝试这种方法的想法扼杀在了摇篮里。
他们指出并发症风险的增加至少部分是由于母体较老的年龄和其它健康因素导致女性试图将辅助生殖技术(APT)放在第一位考虑。
美国疾病控制和预防中心生殖健康卫生科学家Sheree Boulet医生领导了这项研究并指出:“这项研究并没有告诉接受ART后,婴儿出生缺陷风险增加背后的原因。我们的初稿认为原因可能与潜在的生育能力低下相关——导致很多夫妻选择ART,这可能会增加出生缺陷的风险。”
Boulet和她的同事回顾了佛罗里达州从2000年-2010年超过460万的婴儿数据。
4月4日发表在JAMA Pediatrics的报告指出,大约1.4%,粗略的说是65000个婴儿是辅助生殖技术获得的。整体上,每10000个婴儿,有59个使用ART的,至少有1个患者非染色体基因缺陷。大多数不使用ART的女性都小于30岁,接受辅助生殖技术的都至少35岁以上。
即使调整了年龄和其它健康特征后,经ART的婴儿比普通婴儿高出28%的可能性更容易发生出生缺陷。
在多胞胎中,直肠疾病和大肠闭锁/狭窄的风险较未接受ART的婴儿高2.3倍。接受新鲜胚胎移植的婴儿中,患有排卵障碍的女性婴儿出生缺陷的风险增加53%。
在一个接受辅助孵化的女性亚组中,有高出55%的出生缺陷风险。
作者指出,这项研究的缺陷是缺少妊娠产妇未活产婴儿的出生缺陷数据,意味着可能低估了出生缺陷的患病率。也有可能是经ART的婴儿会更加严密的监,导致这类婴儿出生缺陷的检出率更高。
达特茅斯大学医学院妇产科和病理学教授Geisel指出:“尽管这个研究发现了出生缺陷的风险差异,但需要注意的是整体的缺陷率的很低的。未参加此项研究的学者Stern指出,绝大部分ART的婴儿都是正常的。
原始出处:
Reproductive Technology Tied to Higher Risk of Birth Defects,mescape,mar 8 ,2016
Sheree L. Boulet, DrPH, MPH1; Russell S. Kirby,et al, Assisted Reproductive Technology and Birth Defects Among Liveborn Infants in Florida, Massachusetts, and Michigan, 2000-2010 FREE ONLINE FIRST,jama pediatrics,April 04, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#DIA#
31
#试管婴#
26
#PE#
38
文章不错
96
值得学习
89
任何技术都有其时代局限性
102