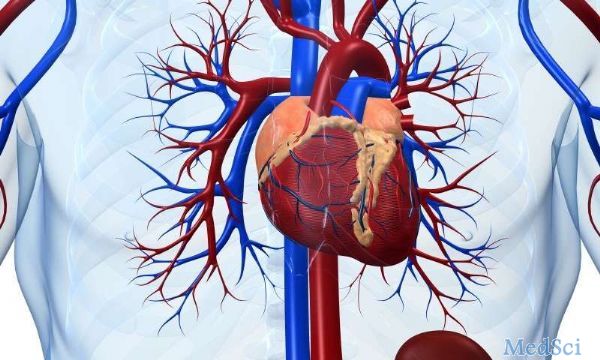
Circulation:CD301b/MGL2+单核巨噬细胞促进自身免疫性心脏瓣膜炎和纤维化
2018-06-11 MedSci MedSci原创
瓣膜性心脏病是一种常见病,最常累积二尖瓣(MV)。尽管二尖瓣疾病(MVD)流行,但其潜在的细胞分子尚不十分清楚。K/B.g7 T细胞受体转基因小鼠会自发形成全身性自身抗体相关的自身免疫病,导致完全穿透性的纤维炎性MVD和关节炎。研究人员利用多参数流式细胞术、细胞内因子染色和免疫荧光染色来区分发炎的MVs中的细胞。用遗传方法研究单核吞噬细胞(MNPs)在该模型中对MVD的贡献度。此外,研究人员还专门
K/B.g7 T细胞受体转基因小鼠会自发形成全身性自身抗体相关的自身免疫病,导致完全穿透性的纤维炎性MVD和关节炎。研究人员利用多参数流式细胞术、细胞内因子染色和免疫荧光染色来区分发炎的MVs中的细胞。用遗传方法研究单核吞噬细胞(MNPs)在该模型中对MVD的贡献度。此外,研究人员还专门建立缺乏CX3CR1或CD301b/MGL2表达的MNPs的K/B.g7小鼠。利用K/B.g7小鼠表达Cx3Cr1-Cre,条件性敲除MNPs中至关重要的炎性分子,包括Fc受体信号转导酪氨酸激酶Syk和细胞黏附分子极晚期抗原4(VLA-4)。建立骨髓嵌合小鼠明确MV中的炎性细胞来源、哪些瓣膜细胞会对促炎性细胞因子——肿瘤坏死因子(TNF)有反应。最后,检测风湿性心脏病患者的样本,以便将本研究发现与人类病理相联系。
MV浸润细胞绝大多数都是MNPs,其表达CX3CR1和CD301/MGL2。在人类风湿性心脏病瓣膜中可见类似的细胞。缺乏CX3CR1表达或敲除了表达CD301b/MGL2的MNPs的K/B.g7小鼠不易罹患MVD。瓣膜浸润的CD301b/MGL2+MNPs表达组织修复分子,包括精氨酸酶-1和抵抗素样α分子。这些MNPs还表达促炎性细胞因子TNF和白介素-6(IL-6);用抗体封闭上述细胞因子可预防MVD。敲除表达CX3CR1的MNPs的Syk可减少其TNF和IL-6的合成,也可预防MVD发生。TNF通过在瓣膜细胞上表达的TNF受体-1发挥作用,增加瓣膜细胞黏附分子-1的表达。条件性敲除表达CXCR1的MNPs的血管细胞黏附分子-1配体VLA-4也可预防MVD。
在K/B.g7小鼠中,CD301b/MGL2+MNPs是自身免疫性MVD的主要致病因子,也存在于人类风湿性心脏病中。在该模型中,Syk、TNF、IL-6、VLA-4和血管细胞黏附分子-1这些炎性细胞因子均可驱动MVD发生。
原始出处:
Lee A. Meier, et al. CD301b/MGL2+ Mononuclear Phagocytes Orchestrate Autoimmune Cardiac Valve Inflammation and Fibrosis. Circulation. June 05,2018. https://doi.org/10.1161/CIRCULATIONAHA.117.033144
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












查了一下,CD301b或者mgl2在人上面目前好像还未检测到表达,请问如果是这样,这项研究的意义有多大?单纯为了发论文?
35
#CD30#
24
#心脏瓣膜#
21
#瓣膜#
27
学习了.长知识
68
学习
66
很好
70
巴巴爸爸红红火火
1