中国患者数据来了!本土卵巢癌PARP抑制剂3期临床研究成果闪耀ESMO
2020-09-20 医谷网 医谷网
2020年9月19日,在刚刚举行的2020年欧洲肿瘤内科学会(ESMO)大会上,由复旦大学附属肿瘤医院妇瘤科主任、妇科肿瘤综合治疗首席专家吴小华教授领衔,全国30余家肿瘤医院联合开展的一项卵巢癌重磅研
2020年9月19日,在刚刚举行的2020年欧洲肿瘤内科学会(ESMO)大会上,由复旦大学附属肿瘤医院妇瘤科主任、妇科肿瘤综合治疗首席专家吴小华教授领衔,全国30余家肿瘤医院联合开展的一项卵巢癌重磅研究“尼拉帕利用于中国铂敏感复发卵巢癌患者维持治疗的3期临床研究NORA”入选完整口头报告(编号LBA29)进行了发布,成为今年唯一一项入选完整口头报告的中国妇瘤研究,受到了国际妇瘤学者的广泛关注。
这是近年来由中国临床专家主导的本土卵巢癌PARP抑制剂临床研究首次以完整口头报告形式在ESMO大会上向国际学者公布核心成果,也是国际上首次对尼拉帕利个体化起始剂量用于铂敏感复发卵巢癌患者的前瞻性临床验证,进一步证实了尼拉帕利个体化起始剂量用于卵巢癌患者维持治疗的临床获益和安全性,同时也是对尼拉帕利在铂敏感复发卵巢癌维持治疗中全人群获益的再次强力印证,有望对中国乃至更多地区的卵巢癌治疗临床实践产生重大影响。
作为国内首个1类新药PARP抑制剂,除了用于铂敏感复发卵巢癌维持治疗外,今年9月,则乐?(尼拉帕利)也已在国内获批用于晚期上皮性卵巢癌、输卵管癌或原发性腹膜癌成人患者对一线含铂化疗达到完全缓解或部分缓解后的维持治疗。至此,尼拉帕利已成为中国及全球唯一获批的无论患者生物标记物状态如何,均能单药用于一线和复发卵巢癌维持治疗的PARP抑制剂,这也意味着卵巢癌一线维持治疗已经进入了全人群时代,真正惠及所有患者。
尼拉帕利再突破,中国卵巢癌维持治疗有了本土证据!
此次登上ESMO完整口头报告的尼拉帕利NORA研究是中国首个PARP抑制剂用于卵巢癌维持治疗的III期随机、双盲、安慰剂对照的研究,是受国家“十三五”“重大新药创制”科技重大专项支持的卵巢癌领域重要研究。
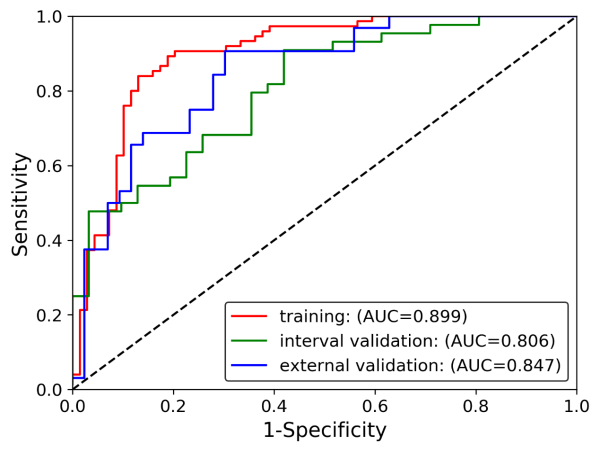
NORA研究代表了PARP抑制剂用于中国铂敏感复发卵巢癌患者的最高级别循证医学证据。研究以2:1的比例随机分配265例患者接受尼拉帕利或安慰剂治疗直至疾病进展。该研究评估了尼拉帕利作为维持治疗的有效性,首要研究终点为通过盲态独立中心评审的无进展生存期(PFS)。除基线体重≥77kg且血小板计数≥150K /μL的患者起始剂量为300 mg外,其余患者均采取起始剂量200 mg的治疗方案。
研究结果显示,接受尼拉帕利维持治疗使总人群中疾病进展或死亡风险降低了68% (PFS HR 0.32; 95% CI, 0.23–0.45; p<0.0001)。相较安慰剂组,接受尼拉帕利治疗显着延长了患者中位无进展生存期(PFS),18.3个月对比5.4个月。令人振奋的是,截止数据分析时,尼拉帕利组有43%的患者无疾病进展,而安慰剂组为13%!此外,在gBRCA突变患者中,接受尼拉帕利治疗的患者疾病进展或死亡风险降低了78%(PFS HR 0.22; 95%CI, 0.12-0.39; p<0.0001);相较于安慰剂组中位PFS为5.5个月,接受尼拉帕利治疗的患者中位PFS尚未达到!在无gBRCA突变组患者中,接受尼拉帕利治疗的患者疾病进展或死亡风险降低了60%(PFS HR 0.40; 95%CI, 0.26-0.61; p<0.0001),尼拉帕利组患者中位PFS为11.1个月,对比安慰剂组3.9个月。
开先河!个体化起始剂量治疗方案有望影响国际临床实践
卵巢癌是影响女性健康的最大威胁之一,死亡率居妇科恶性肿瘤之首。晚期卵巢癌是女性癌症死亡的主要原因,在完成标准一线含铂化疗后,复发率仍高达85%。近年来,PARP抑制剂的问世和应用引领了晚期卵巢癌治疗的变革,卵巢癌的治疗已经逐步进入精准医学时代,目前PARP抑制剂已经成为晚期卵巢癌的标准维持治疗方案。但与此同时,如何个体化地在中国女性中应用PARP抑制剂,在确保疗效的同时减轻不良反应,也成为临床新的关注点。
因此,基于中国国情和以往全球患者的实际应用,NORA研究前瞻性地采用了基于体重和/或血小板计数的个体化起始剂量治疗方案。研究证实,接受尼拉帕利治疗组和安慰剂组的患者中,3级或更高级别的血液学不良事件如中性粒细胞计数降低事件、贫血事件和血小板计数降低事件的发生率分别为20.3%比8.0%,14.7%比2.3%,11.3%比1.1%。
NORA主要研究者吴小华教授表示:“尼拉帕利个体化的起始剂量方案具有显着临床获益和良好的安全耐受性。对于中国本土而言,这项由我们中国临床专家主导的针对中国患者人群开展的‘中国特色’研究,丰富了尼拉帕利维持治疗的中国人群数据,这意味着,更符合国人特征的卵巢癌规范化维持治疗将‘有章可依’。另一方面,面向国际临床实践,NORA研究能够帮助国际专家学者进一步优化PARP抑制剂在卵巢癌患者中的应用,有望改变以往国际标准治疗方式。在个体化精准医疗的指导下,个体化起始剂量的尼拉帕利治疗方案,应被考虑作为全球卵巢癌患者维持治疗的标准临床实践。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#患者数据#
31
#3期临床#
39
#抑制剂#
35
#研究成果#
27
#SMO#
39
#临床研究成果#
30
谢谢分享
79
#ESMO#
33
#PARP#
39
与时俱进,不断进步
71