J Breath Res:呼气分析有望检测呼吸道细菌感染,降低抗生素使用
2016-06-09 佚名 不详

2016年6月8日/生物谷BIOON/--过度使用抗生素让有害细菌有机会进化出威胁健康的耐药性菌株。为了解决这个问题,来自中国浙江大学的研究人员开展一项前瞻性研究,着重关注病人呼气中的生物标志物。这项研究的目标就是开发一种高效的(快速的、准确的、无痛的和花费得起的)测试方法,该方法将有助医生仅当治疗绝对必要时才开出抗生素处方。相关研究结果于2016年6月7日发表在Journal of Breath Research期刊上,论文标题为“Breath analysis for noninvasively differentiating Acinetobacter baumannii ventilator-associated pneumonia from its respiratory tract colonization of ventilated patients”。
在这项研究中,研究人员利用台式仪器分析法作为开发未来的诊断工具的垫脚石。
研究人员在这项初始研究中,研究了重症监护病房中呼吸机相关肺炎患者。在那里,对威胁生命的细菌感染和避免不必要地开出抗生素处方的常见性细菌定植进行区分是至关重要的。
来自浙江大学医学院的Kejing Ying解释道,“为了证实病人是否遭受呼吸道细菌感染,医生当前不得不获取多种不同的样品(血液好痰液),甚至在肺炎情形时,还进行胸部X光检查。”
吸入,呼出
在分析60名志愿者的呼气样品后,研究人员发现呼气中存在的源自鲍曼不动杆菌(Acinetobacter baumannii)的挥发性有机化合物(volatile organic compounds, VOCs)与确诊为细菌性肺炎的患者之间存在潜在有用的关联。
Ying补充道,“我们面临的挑战是很多VOCs并不是一种病原体独有的。
最终,研究人员希望这项研究将导致人们开发出一种获得批准的非侵入性测试方法,以便能够对下呼吸道细菌感染进行早期预警。(生物谷 Bioon.com)
本文系生物谷原创编译整理,欢迎转载!点击 获取授权 。更多资讯请下载生物谷APP。
Breath analysis for noninvasively differentiating Acinetobacter baumannii ventilator-associated pneumonia from its respiratory tract colonization of ventilated patients
doi:10.1088/1752-7155/10/2/027102
Jianping Gao1, Yingchang Zou2, Yonggang Wang1, Feng Wang1, Lang Lang2, Ping Wang2, Yong Zhou3 and Kejing Ying
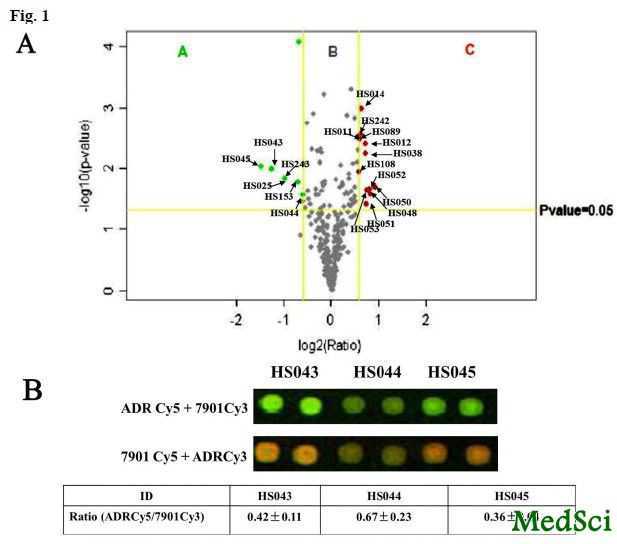
A number of multiresistant pathogens including Acinetobacter baumannii (A. baumannii) place a heavy burden on ventilator-associated pneumonia (VAP) patients in intensive care units (ICU). It is critically important to differentiate between bacterial infection and colonization to avoid prescribing unnecessary antibiotics. Quantitative culture of lower respiratory tract (LRT) specimens, however, requires invasive procedures. Nowadays, volatile organic compounds (VOCs) have been studied in vitro and in vivo to identify pathogen-derived biomarkers. Therefore, an exploratory pilot study was conceived for a proof of concept that the appearance and level of A. baumannii-derived metabolites might be correlated with the presence of the pathogen and its ecological niche (i.e. the infection and colonization states) in ICU ventilated patients.
Twenty patients with A. baumannii VAP (infection group), 20 ventilated patients with LRT A. baumannii colonization (colonization group) and 20 ventilated patients with neurological disorders, but without pneumonia or A. baumannii colonization (control group) were enrolled in the in vivo pilot study. A clinical isolate of A. baumannii strains was used for the in vitro culture experiment. The adsorptive preconcentration (solid-phase microextraction fiber and Tenax® TA) and analysis technique of gas chromatography–mass spectrometry were applied in the studies.
Breath profiles could be visually differentiated between A. baumannii cultivation in vitro and culture medium, and among in vivo groups. In the in vitro experiment, nine compounds of interest (2,5-dimethyl-pyrazine, 1-undecene, isopentyl 3-methylbutanoate, decanal, 1,3-naphthalenediol, longifolene, tetradecane, iminodibenzyl and 3-methyl-indene) in the headspace were found to be possible A. baumannii derivations. While there were eight target VOCs (1-undecene, nonanal, decanal, 2,6,10-trimethyl-dodecane, 5-methyl-5-propyl-nonane, longifolene, tetradecane and 2-butyl-1-octanol) exhibiting characteristics of A. baumannii VAP derivations. The selected VOC profile in vivo could be adopted to efficiently differentiate the presence of LRT A. baumannii from its absence, and LRT A. baumannii infection from its colonization (AUC = 0.89 and 0.88, respectively).
It is not feasible to simply transfer the metabolic biomarkers from the in vitro condition to in vivo. The direct detection of exhaled A. baumannii-derived VOCs may be adopted for an early alert of the LRT bacterial presence in ventilated ICU patients, and even in different parasitic states of A. baumannii (i.e. infection and colonization). However, further refinement and validation are required before its clinical use.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#抗生素使用#
32
应该这样
120
这个不错
120
#细菌感染#
33
#呼吸道#
34
#Breath#
31