JACC:二尖瓣环钙化患者经导管二尖瓣置换术的预后研究
2018-04-25 MedSci MedSci原创
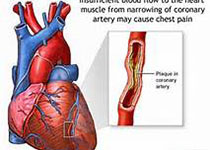
对于严重的二尖瓣环钙化(MAC)病人,外科的二尖瓣置换术的风险较高,目前在世界范围内,有数例MAC患者成功接受了经导管二尖瓣置换术(TMVR),并建立了MAC患者的TMVR注册中心。本研究的目的旨在评估该数据库中接受TMVR治疗的MAC患者的1年临床预后。本研究共纳入了106名接受有TMVR的MAC患者,患者的平均年龄为73 ± 12岁,女性占68%,平均的胸外科医师学会评分为15.3 ± 11.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#置换#
38
#二尖瓣置换术#
40
#经导管二尖瓣置换术#
46
#JACC#
43
#ACC#
25
#二尖瓣#
29
#经导管#
28
#置换术#
32
#二尖瓣环钙化#
28
谢谢分享学习
65