Nat Commun:m6A RNA甲基化识别蛋白YTHDF1在低氧适应和非小细胞肺癌发生发展中的重要功能
2019-11-04 佚名 细胞
《Nature Communications》期刊在线发表了陈勇彬学科组的最新研究成果“YTHDF1 links hypoxia adaptation and non-small cell lung cancer progression”。该工作揭示了YTHDF1在低氧适应和非小细胞肺癌发生发展中的重要功能和分子调控机理。
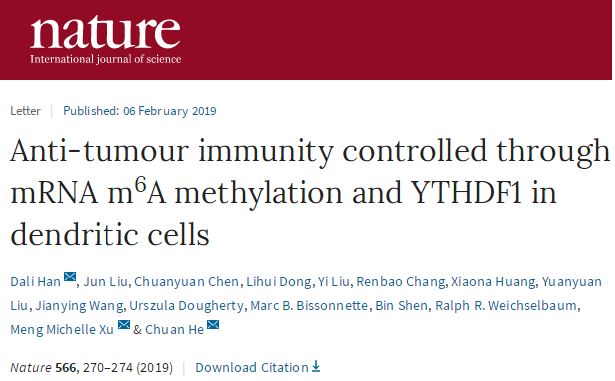
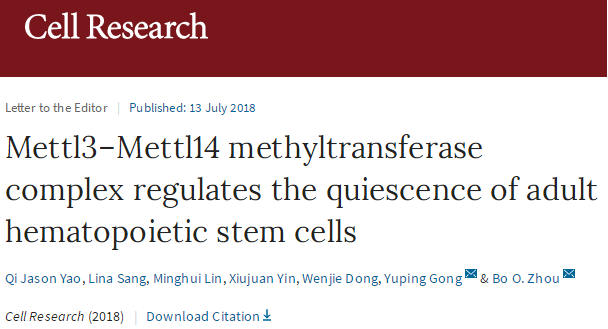
陈勇彬学科组前期与吴东东学科组合作,利用进化生物学的方法,筛选得到一系列青藏高原家养哺乳动物低氧适应的关键新分子,并发现许多已报道的肿瘤明星基因在高原家养哺乳动物中受到正选择,提示低氧适应新基因在低氧实体瘤中具有潜在重要功能。研究发现YTHDF1作为m6A修饰后的RNA结合蛋白家族成员之一,在高原家养哺乳动物中低表达,而在正常肺上皮细胞中抑制其表达可以抵抗低氧诱导的细胞凋亡。深入研究发现,YTHDF1在非小细胞肺癌肿瘤组织和细胞系中均高表达,其在常氧条件下通过加速CDK2和CDK4等细胞周期蛋白的表达来促进肿瘤细胞的增殖;而在铂类药物为主的化疗压力环境下,由于YTHDF1高表达促进了Keap1蛋白的表达,导致Nrf2转录因子的迅速降解和下游耐药基因AKR1C1的沉默,因此肿瘤患者对化疗更敏感且总生存时间更长。
该研究表明,利用极端环境生存的非模式动物基因组,通过进化生物学方法筛选低氧适应的相关基因,可以为低氧实体瘤新生物标志物的挖掘提供新的研究方法,提示交叉学科在未来医学生物学研究领域具有重要的应用前景。
陈勇彬学科组石玉林博士,中南大学湘雅医院范松青教授和昆明医科大学吴梦鸽硕士为本文的共同第一作者,陈勇彬研究员,杨翠萍研究员和吴东东研究员为共同通讯作者。该工作得到了中科院上海生科院季红斌、周虎、徐书华研究团队及中山大学左志向教授的支持,中科院上海生科院李党生与昆明动物所施鹏及周巨民研究员积极参与了论文的讨论。该工作由国家重点研发计划(2016YFA0100900)和中科院先导项目(XDB13000000)及国家自然科学基金等项目资助。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#非小细胞#
29
#发生发展#
33
#Nat#
44
#COMMUN#
28
#m6A#
45