Nat biotech:超级CAR-T细胞让肿瘤完全消失!
2019-07-10 不详 网络
人类肿瘤治疗史上的里程碑无疑一定有一座是肿瘤免疫疗法的。而肿瘤免疫疗法的主要两大领域,细胞治疗以及以PD1/PDL1为代表的免疫检查点抑制剂都在飞速发展。目前,已经有5种抗PD1/PDL1抗体药物上市,包括默沙东的Keytruda、百时美施贵宝的Opdivo、罗氏的Tecentriq、辉瑞和德国默克生产的Bavencio以及阿斯利康生产的Imfinzi。 而以CAR-T为代表的细胞免疫疗
人类肿瘤治疗史上的里程碑无疑一定有一座是肿瘤免疫疗法的。而肿瘤免疫疗法的主要两大领域,细胞治疗以及以PD1/PDL1为代表的免疫检查点抑制剂都在飞速发展。目前,已经有5种抗PD1/PDL1抗体药物上市,包括默沙东的Keytruda、百时美施贵宝的Opdivo、罗氏的Tecentriq、辉瑞和德国默克生产的Bavencio以及阿斯利康生产的Imfinzi。

而以CAR-T为代表的细胞免疫疗法目前也已经有两款上市,即诺华的Kymriah以及Kite公司(现已被吉列德公司收购)的Yescarta。
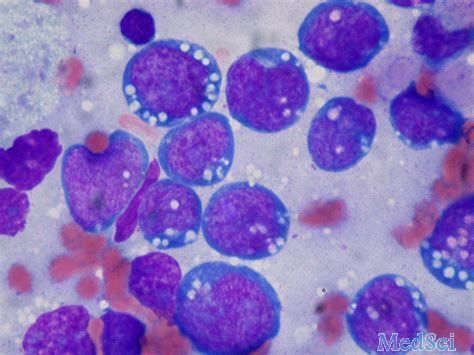
然而,目前上市的细胞免疫疗法Kymriah以及Yescarta都是针对血液肿瘤的,对于实体肿瘤而言,目前的CAR-T仍然还面临许多困难,比如治疗实体瘤效果不佳,不能够有效地浸润到肿瘤组织内部,CAR-T细胞生存时间不长等等。
▲研究者们在国际著名期刊《自然-生物技术》杂志上面发表的文章(图片来自Nature)
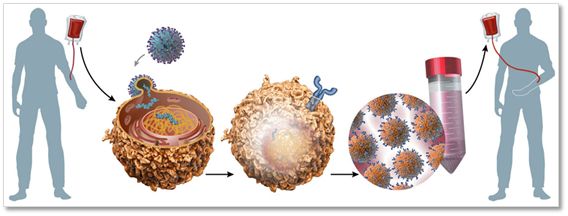
3月5日,最新一期国际著名学术期刊《自然-生物技术》在线发表了一篇关于免疫治疗肿瘤的重磅文章,一组来自日本的科学家团队通过将IL-17以及CCL-19基因转入CAR-T细胞制备出能够有效杀伤肿瘤的“超级CAR-T细胞”,能够让患有肿瘤的小鼠几乎100%生存,这种细胞在体内存活时间更长并且能够有效地帮助DC细胞以及T细胞浸润到肿瘤组织内部一起杀伤肿瘤【1】。
▶7x19◀
研究者们把这项创新的CAR-T技术叫做“7x19CAR-T细胞”。
主要是在以往的CAR-T基础之上将IL-17以及CCL19添加进去改造而成。那么,为何要添加IL-17以及CCL19这两个基因呢?
原来,以往的研究发现,淋巴器官之中的纤维网状细胞(Fibroblastic reticular cells)分泌的IL-17和CCL19能够将外围的T细胞和DC细胞有效地招募过来,以便维持T细胞集中的区域(T cell zone)【2,3】。因此,研究者们就受到这个启发,期望将IL-17和CCL19也装到CAR-T细胞之中,看能不能在治疗肿瘤的同时招募更多的T细胞以及DC细胞来肿瘤组织中一起杀伤肿瘤。
研究者们还真是善于学习,这正应了我国的名言,所谓“师夷长技以制夷”,向相关的细胞学习,然后再把相同的原理用到CAR-T身上。
那么,研究者们是怎么改造的呢?
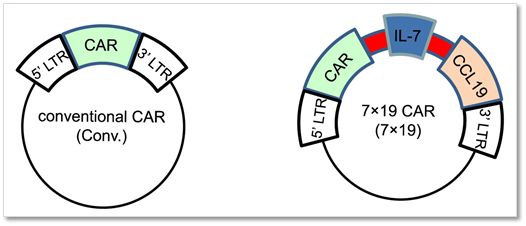
▲研究者们将表达IL-17以及CCL19的基因构建到CAR质粒载体中,左图表示正常的表达CAR(嵌合抗原受体)的质粒,右图表示CAR-IL17-CCL19共表达质粒,其中CAR、IL-17以及CCL19之间用2A肽连接(图中红色区域)
这简单,将CAR-IL17-CCL19全部构建到一个质粒中共同表达就行了,其中,这几个元件之间采用2A短肽连接,表达之后就在细胞中自动分裂成三个,各自行使各自的功能了。
▶T细胞的渗透◀
那么,研究者们的设计是不是能够让他们如愿以偿呢?
答案是肯定的。
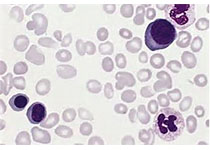
研究者们采用改造之后的7x19CAR-T细胞治疗小鼠的肿瘤,然后把肿瘤组织切片,用免疫荧光技术来观察肿瘤组织中的T细胞和DC细胞的数量,结果显示,7x19CAR-T细胞治疗之后,T细胞及DC细胞明显增多,而采用常规CAR-T治疗的小鼠,其肿瘤组织中T细胞和DC细胞很少,几乎都在肿瘤组织的外缘。换句话说,这相当于帮助T细胞渗透进入实体瘤组织中。
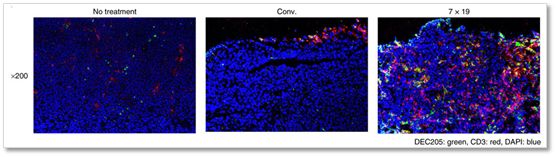
▲研究者们采用改造之后的7x19CAR-T细胞治疗小鼠的肿瘤,然后把肿瘤组织切片,用免疫荧光技术来观察肿瘤组织中的T细胞和DC细胞的数量;图中的红色部分表示T细胞、绿色表示浸润性DC细胞,可以看到,7x19CAR-T细胞治疗之后,T细胞及浸润性DC细胞明显增多(右小图)
这说明,经过改造之后的7x19CAR-T细胞能够帮助身体中的T细胞以及DC细胞有效地浸润到肿瘤组织内部,进而对肿瘤细胞进行杀伤。
实际上,这解决了目前CAR-T治疗实体肿瘤最大短板之一:CAR-T细胞无法有效地进入实体瘤组织内部,而绝大多数都被挡在肿瘤组织外围,造成CAR-T细胞无法和肿瘤细胞直接接触进而杀伤肿瘤的困境。
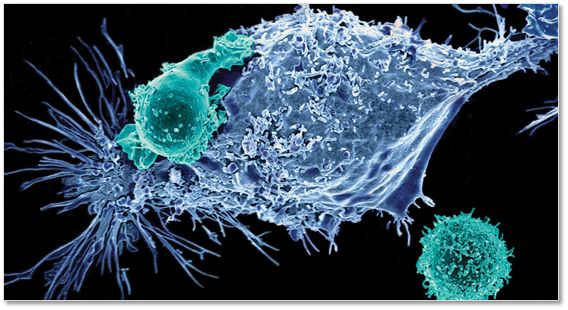
确实,若是CAR-T细胞无法直接和肿瘤细胞接触,那么,它们又如何能够杀伤得了肿瘤细胞呢?而实体肿瘤常常较为致密,造成CAR-T常常被挡在外围,在空间上不能够有效地接近肿瘤细胞。
▶消灭小鼠所有肿瘤◀
当然,作为一款治疗肿瘤的改进创新方法,虽然把牛皮吹上了天,但要是没有什么效果的话,那也没有什么应用价值。
对于治疗方法而言,关键是看效果。
那么,究竟这种超级CAR-T细胞的治疗肿瘤的效果如何呢?
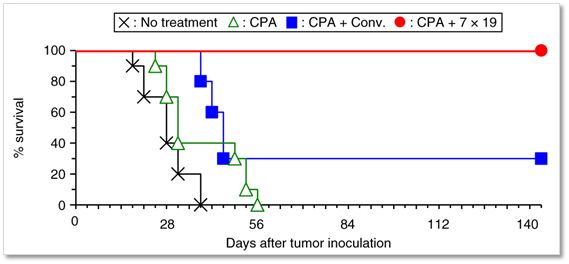
▲研究者们采用改造之后的7x19CAR-T细胞治疗小鼠肥大细胞癌,结果几乎100%的小鼠都能够存活(红色线),而常规CAR-T治疗存活率只有30%左右(蓝色线);CPA:环磷酰胺(cyclophosphamide),一种免疫抑制剂(图片来自Nature)
可以说,7x19CAR-T治疗肿瘤的效果是相当让人惊喜的,所有的荷瘤小鼠都存活了下来,生存率达到100%,而采用常规CAR-T疗法的肿瘤小鼠生存率只有30%左右。
当然,不要以为研究者们只实验了一种少见的肿瘤,对于其他的肿瘤比如肺癌、胰腺癌也一样,7x19CAR-T治疗之后,小鼠生存率几乎都达到100%。
尽管是小鼠实验,这样的结果已经让人非常满意了。
不但如此,研究者们还继续探讨了单独使用IL-7和单独使用CCL19均不能够有效地提高CAR-T的杀伤能力,只有IL-7和CCL19合在一起时才能够发挥超强肿瘤杀伤作用。
并且,研究者们进一步观察到,7x19 CAR-T输入荷瘤小鼠之后,主要是存在于肿瘤组织部位,而不会存在于身体的其他部位,这说明这一疗法的安全性较高。
期待这一疗法在未来能够有更加深入的研究。
参考资料:
1. IL-7 and CCL19 expression in CAR-T cellsimproves immune cell infiltration and CAR-T cell survival in the tumor.2018.
2. Link, A. et al. Fibroblastic reticularcells in lymph nodes regulate the homeostasis
of naive T cells. Nat. Immunol. 8,1255–1265 (2007).
3. Luther, S.A. et al. Differing activitiesof homeostatic chemokines CCL19, CCL21,
and CXCL12 in lymphocyte and dendritic cellrecruitment and lymphoid neogenesis.
J. Immunol. 169, 424–433 (2002).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Bio#
23
#TEC#
24
#Nat#
29
#Biotech#
35
#CAR-#
25