ESMO速递:晚期食管鳞癌研究进展,免疫治疗再下一城
2019-10-13 佚名 肿瘤资讯
2019年欧洲肿瘤内科学会(ESMO)年会于西班牙巴塞罗那举行,该会议是欧洲最负盛名和最具影响力的肿瘤学会议,会议期间有大量肿瘤临床治疗相关的研究结果公布,为推动肿瘤诊疗发挥巨大作用。在本次ESMO大会上,肿瘤免疫治疗(IO)仍是会议的热点内容。在消化道肿瘤领域,特别是食管癌的治疗方面,今年的重磅研究当属ATTRACTION-3研究,这是首个证实无论PD-L1是否表达阳性,PD-1单抗对比化疗二线
2019年欧洲肿瘤内科学会(ESMO)年会于西班牙巴塞罗那举行,该会议是欧洲最负盛名和最具影响力的肿瘤学会议,会议期间有大量肿瘤临床治疗相关的研究结果公布,为推动肿瘤诊疗发挥巨大作用。在本次ESMO大会上,肿瘤免疫治疗(IO)仍是会议的热点内容。在消化道肿瘤领域,特别是食管癌的治疗方面,今年的重磅研究当属ATTRACTION-3研究,这是首个证实无论PD-L1是否表达阳性,PD-1单抗对比化疗二线治疗食管鳞癌可以显着改善OS的Ⅲ期临床研究。其结果一经发布便吸引了众多临床专家的关注。未来,免疫治疗或将成为二线晚期食管鳞癌标准治疗选择之一。
ESMO重磅:晚期食管鳞癌治疗新突破,免疫治疗或将成为晚期食管鳞癌二线治疗新选择
此次ESMO大会上,晚期食管鳞癌的治疗取得了新的突破,成为了大会学术焦点之一。会上公布了ATTRACTION-3的研究结果,是首个证实无论PD-L1是否表达阳性,免疫治疗在食管鳞癌二线治疗中较化疗显着改善OS的Ⅲ期临床研究。ATTRACTION-3研究是一项多中心、随机、开放的Ⅲ期研究,入组年龄20岁及以上,病理确诊为鳞癌或腺鳞癌的不可切除的晚期或复发性食管癌患者。患者既往接受过5-FU和铂类为基础的一线化疗后不可耐受或疾病进展。入组人群按1∶1随机接受纳武利尤单抗或研究者选择的化疗治疗。主要研究终点为总生存(OS),次要研究终点包括研究者评估的客观缓解率(ORR)、无进展生存期(PFS)、疾病控制率(DCR)和疗效持续时间(DOR)等。
研究共入组419例患者,其中96%(401/419)为亚洲患者。在随访了至少17.6个月以后,主要研究终点OS获益分析显示,纳武利尤单抗组对比化疗组降低了23%的死亡风险,中位OS增加了2.5个月。纳武利尤单抗治疗组12个月的OS率为47%。亚组分析显示,无论患者PD-L1表达水平如何,均可以获得OS获益。
安全性分析,纳武利尤单抗组对比化疗组显示出更好的安全性,3~4级治疗相关不良反应(TRAE)发生率较化疗组降低2/3(18% vs 63%)。生活质量评估显示,纳武利尤单抗对比化疗,在治疗过程中观察到HRQoL的显着改善。
延伸讨论
全球范围内,食管癌是第7大常见肿瘤,也是第6大癌症相关死亡原因[1],患者预后较差,晚期食管癌患者5年生存率不超过8%[2,3]。中国是食管癌大国,我国食管癌发病率和死亡率均居全球前列。在我国,食管鳞癌是最主要的组织学类型,约占所有食管癌的90%。
食管癌患者因缺乏有效的治疗策略,总体的生存和生活质量差。目前晚期食管癌患者的治疗以化疗为主,但严重缺乏有效的系统性化疗方案。5-FU和铂类双药化疗是晚期食管鳞癌较常用的一线化疗方案。在二线治疗阶段,可以根据患者的获益风险评估决定是否接受单药化疗,推荐的二线化疗方案为紫杉醇或多西他赛单药治疗,常引发严重的血液学、胃肠道和神经毒性,且疗效有限,患者的长期预后较差。靶向治疗方面,抗HER2靶向治疗仅适用于较为少见的食管腺癌且表达阳性的患者。对于食管鳞癌目前尚无明确验证疗效的靶向方案。此外,由于食管癌发病部位特殊,多数患者病程中合并饮食困难、严重营养不良等情况,影响其生活质量。综上所述,对于晚期食管癌、尤其是鳞癌患者的治疗存在巨大的未被满足的需求。
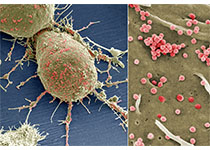
免疫检查点抑制剂的抗肿瘤疗效已经在多种类型的鳞癌患者中得到证实,包括食管鳞癌、头颈鳞癌、肺鳞癌和肛门鳞癌。免疫检查点抑制剂,如PD-1单抗的作用机制主要为通过阻断PD-1受体与配体的结合,增加T细胞的抗肿瘤活性来实现杀伤肿瘤的作用。此独特的作用机制或将使免疫治疗成为晚期食管癌新的治疗选择。
免疫治疗在食管癌中已崭露头角,更多研究值得期待
免疫检查点抑制剂在晚期食管鳞癌中已经进行了多项研究探索。在晚期食管癌三线治疗上,Ⅱ期临床ATTRACTION-1研究,在既往接受过5-FU为基础、铂类为基础和紫杉醇为基础化疗后进展的晚期食管鳞癌中,证实了免疫治疗可耐受的安全性和有前景的疗效。Ⅱ期临床研究KEYNOTE-180也初步确认了免疫三线及以上治疗PD-L1表达阳性晚期食管癌的疗效和安全性。
在晚期食管癌二线治疗上,多队列ⅠB期研究KEYNOTE-028,初步证实了免疫治疗二线用于PD-L1阳性晚期食管癌的疗效和安全性。ATTRACTION-3研究是首个证实免疫治疗用于晚期食管鳞癌二线治疗较化疗有显着OS获益的Ⅲ期临床研究。其研究目的在于对比PD-1单抗和化疗在化疗后进展或不可耐受的不可切除晚期或复发性食管鳞癌中的疗效。该研究结果观察到显着的生存获益,且无论PD-L1表达水平,其安全性及生活质量数据显着优于化疗。免疫治疗有望成为晚期食管鳞癌无论PD-L1表达阳性的患者的二线治疗标准方案新选择。
此外,免疫检查点抑制剂在晚期一线及可手术切除的食管鳞癌治疗中也开展了相关探索:包括晚期一线治疗中开展的免疫联合化疗的KEYNOTE-590研究和免疫联合化疗或双免疫治疗的CheckMate-648研究,以及免疫治疗单药用于可手术切除食管鳞癌辅助治疗的CheckMate-577研究。后两项研究均有中国有多家中心参与,结果值得期待。
小结
中国是食管鳞癌大国,目前晚期食管鳞癌治疗仍以化疗为主,且疗效有限,毒副作用明显。此次ESMO 研究上公布的ATTRACTION-3主要研究数据显示PD-1单抗对比化疗用于经治晚期食管鳞癌,无论患者的PD-L1表达水平,均可带来显着的生存获益,且显示出良好的安全性,显着改善患者的生活质量。基于这一研究结果,免疫治疗有望成为经治晚期食管鳞癌二线治疗的新选择。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#SMO#
29
#ESMO#
28
#研究进展#
20
#食管#
28
#鳞癌#
41
#晚期食管鳞癌#
31