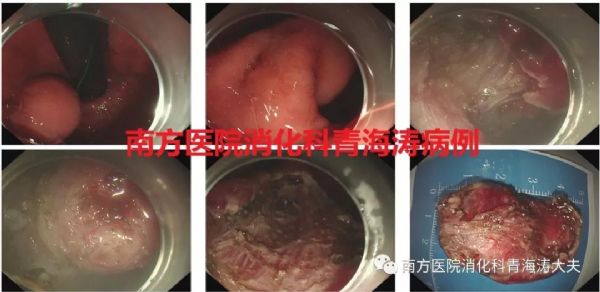
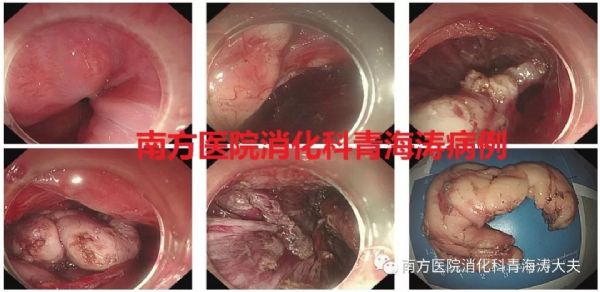
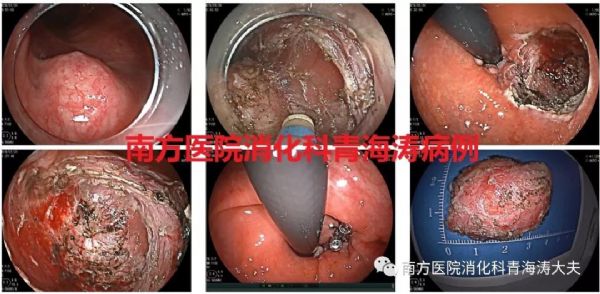
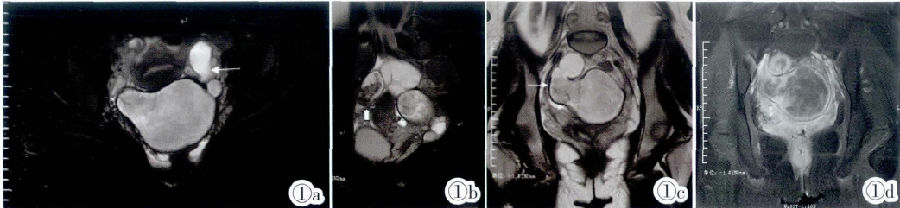
病例:巨大胃肠间质瘤内镜下切除术
2019-06-19 青海涛 南方医院消化科青海涛大夫
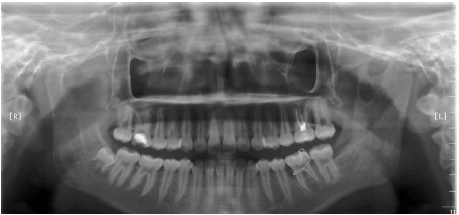
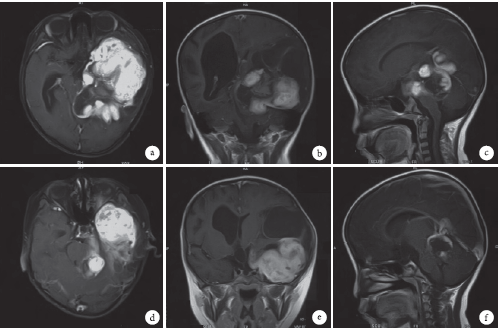
患者陈某,男,54岁,外院胃镜、超声胃镜提示胃底近穹隆部可见大小约3.5cm黏膜下肿物(壁间型),切除后观察大小约5 cm *4 cm。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#内镜下切除#
54
#切除术#
42
#内镜#
46
#间质瘤#
47
学习近平18日给北京体育大学2016级研究生冠军
103