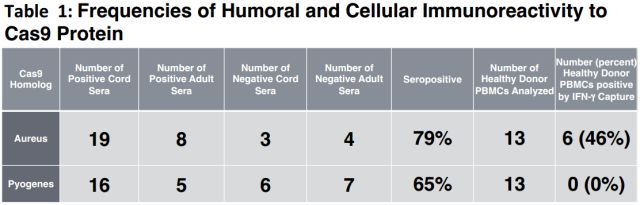
BioRxiv:啥!?上帝的剪刀手CRISPR/Cas9或在人体无效,斯坦福大学科学家在七成人体内发现Cas9同源蛋白抗体
2018-01-09 代丝雨 奇点网
2017年可谓是基因治疗大放异彩的一年,在镰状细胞病、脊髓性肌萎缩症、血友病等绝症上,基因治疗屡斩奇功,不得不让人心生期待。而在基因治疗大家庭里,CRISPR更是让科学家寄予厚望。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Bio#
21
#RISPR/Cas9#
49
斯坦福大学科学家的成果.
62
#CRISPR#
31
#CRISPR/Cas9#
35
#Cas9#
28
#Cas#
22
学习了新知识
47
学习了很有用
41
学习了.获益匪浅!感谢分享
44