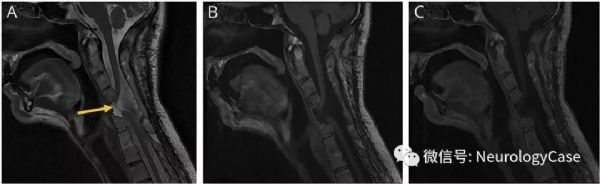
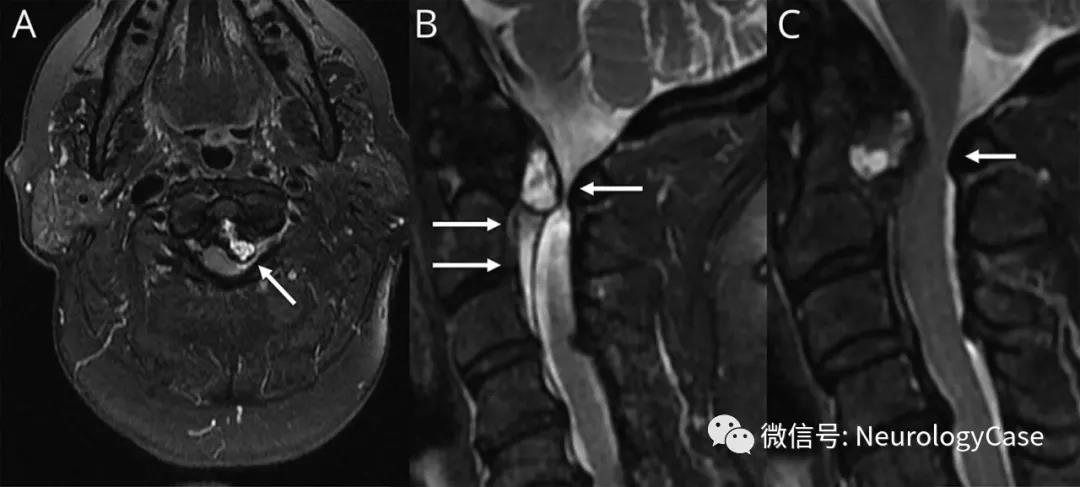
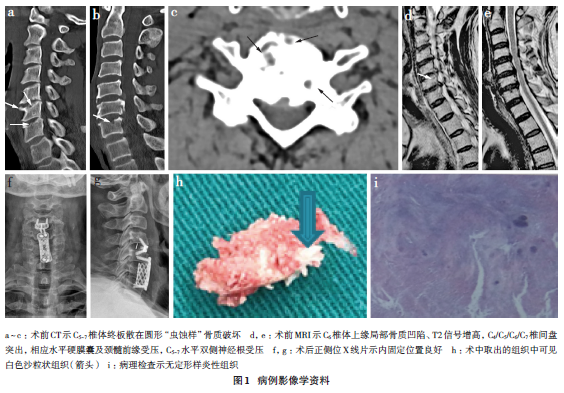
Neurology:颈椎椎体次全切除后出现脊髓疝
2019-12-24 zyx整理 神经科病例撷英拾粹
48岁男性,表现为逐渐加重的全身疼痛。患者既往有复杂的颈椎畸形行C2-T4前后器械融合。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#脊髓疝#
46
#Neurol#
28
#椎体#
48
#疝#
33
很好的学习机会
87
谢谢了,学习
85