Circulation:COVID-19感染患者的心功能障碍!
2020-08-01 QQY MedSci原创
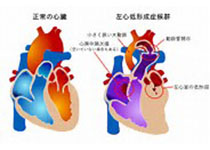
COVID-19感染时,大部分患者的左室收缩功能正常,但左室舒张功能和右心室功能受损。肌钙蛋白升高和临床分级较差的患者的右心室功能往往也较差。
Szekely等连续对100例确诊为COVID-19感染的患者在入院24小时内进行了完整的超声心动图评估,并与参考值进行比较。超声心动图检查项目包括左心室(LV)收缩和舒张功能、瓣膜血流动力学和右心室(RV)评估,以及肺超声。并在患者临床情况恶化的情况下进行第二次检查。
32例患者的初次超声心动图检查正常。最常见的心脏病变是右心室扩张和功能障碍(39%),其次是左心室舒张功能不全(16%)和左心室收缩功能障碍(10%)。与肌钙蛋白正常或病情较好的患者相比,肌钙蛋白升高(20%)或病情较差的患者的左室收缩功能无明显差异,但右心室功能较差。20%的患者出现病情恶化。在病情恶化的患者中,随访过程中最常见的异常是右心室功能恶化(12例)、其次是左心室收缩和舒张功能恶化(5例)。12例心衰患者中有5例发生股深静脉血栓。
COVID-19感染时,大部分患者的左室收缩功能正常,但左室舒张功能和右心室功能受损。肌钙蛋白升高和临床分级较差的患者的右心室功能往往也较差。在随访过程中病情恶化的患者中,伴有或不伴有深静脉血栓形成的急性右心室功能障碍更为常见。
原始出处:
Yishay Szekely, et al. Spectrum of Cardiac Manifestations in COVID-19. Circulation. 2020;142:342–353
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











优秀
62
对
84
优秀
75
#功能障碍#
36
#心功能#
60
赞
67
优秀
82
牛
33