JAMA Oncol:注意!口服化疗药物治疗时,联用质子泵抑制剂,会导致更差的生存!
2016-10-19 MedSci MedSci原创
卡培他滨是常使用的口服化疗药之一,与其他口服药物一起服用时,卡培他滨可能会受到药物间相互作用影响,不利于药物的吸收。 本研究的目的是,探究如质子泵抑制剂(PPIs)等胃酸抑制剂,是否会对卡培他滨的疗效不利。 研究纳入了545例ERBB2/HER2阳性的性转移性食管癌(GEC)患者,按1:1随机分为卡培他滨和奥沙利铂(CapeOx)伴或不伴拉帕替尼。比较使用或没有使用PPIs患者的无进展
卡培他滨是常使用的口服化疗药之一,与其他口服药物一起服用时,卡培他滨可能与其他药物相互作用影响,不利于药物的吸收。
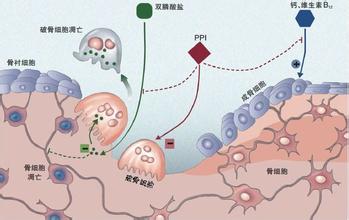
本研究的目的是,探究如质子泵抑制剂(PPIs)等胃酸抑制剂,是否会对卡培他滨的疗效不利。
研究纳入了545例ERBB2/HER2阳性的性转移性食管癌(GEC)患者,按1:1随机分为卡培他滨和奥沙利铂(CapeOx)伴或不伴拉帕替尼。比较使用或没有使用PPIs患者的无进展生存期(PFS)和总生存(OS)情况。
在这545例GEC患者(中位年龄60岁;406例[ 74% ]男性)中,229例接受PPIs (42.0%)治疗,在两个治疗组的分布是类似的。
安慰剂组,PPI治疗的患者与未使用PPI治疗的患者相比,有更差的中位PFS4.2 vs 5.7个月 (HR, 1.55; 95% CI, 1.29-1.81, P < 0.001),更差的OS 9.2 vs 11.3个月(HR, 1.34; 95% CI, 1.06-1.62; P =0 .04),及疾病控制率(83% vs 72%; P =0 .02)。
校正年龄、种族、疾病分期、性别后,多变量分析显示,PPI治疗的患者有更差的PFS(HR, 1.68; 95% CI, 1.42-1.94; P < .001)和OS(HR, 1.41; 95% CI, 1.11-1.71; P = .001)。
使用CapeOx+拉帕替尼治疗的患者,PPI对PFS(HR, 1.08; P = .54)和OS(HR, 1.26; P = .10)的影响更小。不过多因素分析仍显示,PPI治疗会对这组患者的OS产生不利影响。
质子泵抑制剂可能通过胃内PH值的改变,影响药物的溶解和吸收,进而导致患者的生存变差。
原始出处:
Michael P. Chu,et al.Association of Proton Pump Inhibitors and Capecitabine Efficacy in Advanced Gastroesophageal Cancer.JAMA Oncol. Published online October 13, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#质子泵#
36
#抑制剂#
35
#Oncol#
36
学习了。谢谢
83
#化疗药物#
42
#化疗药#
32
值得关注。学习了。
69