BMC Infect Dis:CMV基因组变异与有症状的感染和听力损失相关性研究
2020-01-01 AlexYang MedSci原创
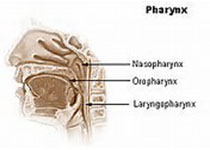
新生儿巨细胞病毒感染(cCMV)是最常见的先天性感染,并且是长期神经和感觉后遗症的主要诱因,其中最常见的为感官听力损失(SNHL)。尽管已有大量的研究,鉴定疾病风险增加的CMV感染儿童的临床或者实验室标记仍旧还没有鉴定。最近,有研究人员进行了病毒全基因组测序(NGS)来探索病毒多样性和特定的病毒变异与有症状的感染和SNHL相关性情况。研究包括了从30个从婴儿尿液中提取的CMV DNA样。研究人员对
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BMC#
45
#Dis#
41
#CMV#
58
#相关性#
40
#听力#
33
#变异#
28