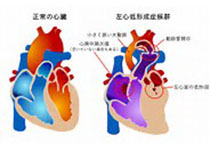
阜外研究称:肥厚型心肌病猝死高危患者安装ICD可救人一命,有猝死家族史者更适合
2019-03-30 闫丽荣,陈柯萍,戴研,等 中国循环杂志
阜外医院陈柯萍、闫丽荣等发表目前国内较大样本量研究结果显示,肥厚型心肌病猝死高危患者安装ICD的恰当治疗率高,植入相关并发症少。
阜外医院陈柯萍、闫丽荣等发表目前国内较大样本量研究结果显示,肥厚型心肌病猝死高危患者安装ICD的恰当治疗率高,植入相关并发症少。
研究观察了38例2011年~2017年在阜外医院植入ICD作为一级预防的肥厚型心肌病猝死高危患者。平均随访29个月。
36.8%患者接受≥1次的 ICD 恰当治疗。一级预防患者中 ICD 恰当治疗率为 13.3%/年,高于既往研究。
研究者分析原因,本研究中50% 的患者有不明原因晕厥史,明显高于既往研究(30%~40%)。
如何筛选出心原性猝死高危患者并植入 ICD 作为一级预防非常重要,也面临巨大挑战。
本研究显示,ICD 恰当治疗患者中,有心原性猝死家族史的比例显著高于无ICD 恰当治疗患者,多因素回归提示心原性猝死家族史是 ICD 恰当治疗的独立预测因子(HR=11.8)。
本研究随访期间,随访期间有 4 例(10.5%)患者接受 ICD 不恰当治疗。2 例(5.3%)患者发生 ICD 植入相关并发症,随访期间无死亡事件发生。
不恰当治疗的主要原因为室上性快速心律失常导致的不恰当识别和导线故障。
本研究进一步分析发现,在本研究人群中,2014年ESC指南肥厚型心肌病 Risk-SCD 模型适用性不佳。
2014年ESC指南提出了肥厚型心肌病Risk-SCD 模型,该模型是在一项多中心回顾性研究(n=3 675)中建立并验证的肥厚型心肌病患者心原性猝死风险评估模型。
本研究显示,肥厚型心肌病 Risk-SCD 模型的敏感度和特异度均较低。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ICD#
41
#高危患者#
36
#家族史#
39
#救人#
38
#肌病#
28