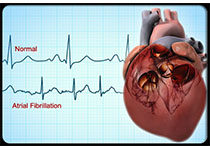
JAHA:NOACs与华法林对房颤患者痴呆发生的影响
2019-06-01 不详 MedSci原创
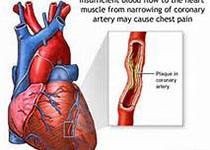
目前,非维生素K拮抗剂口服抗凝药(NOACs)能否减轻房颤患者的痴呆进展尚不清楚。本研究的目的旨在比较和评估NOACs和华法林对房颤患者痴呆进展的影响。本研究纳入了丹麦国家数据库中33617名接受口服抗凝药治疗的房颤患者,其中11052名患者年龄在60-69岁,13237名年龄在70-79岁,9238名年龄≥80岁。有约60%的患者服用NOACs治疗,40%的患者服用华法林。经过平均3.4年时间的
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#AHA#
27
#ACS#
35
#NOAC#
33
#NOACs#
40
#房颤患者#
0
老年人痴呆何药可用??
48