DDW 2016:超声内镜(EUS)进展
2016-06-09 MedSci MedSci原创
5月21-24日,2016 消化疾病周(DDW)在美国圣迭戈召开,首都医科大学附属北京友谊医院消化科张澍田教授和李鹏教授就年会中有关超声内镜(EUS)相关进展进行介绍,与同道分享。 迈克尔(Michael)教授介绍了超声内镜在腹腔血管疾病的临床应用。其通过多则病例,展示了EUS在这一方面的价值。第1例患者因上消化道出血就诊,反复行胃镜检查均未显示出血灶,EUS检查显示,食管明显曲张静脉,
5月21-24日,2016 消化疾病周(DDW)在美国圣迭戈召开,首都医科大学附属北京友谊医院消化科张澍田教授和李鹏教授就年会中有关超声内镜(EUS)相关进展进行介绍,与同道分享。

迈克尔(Michael)教授介绍了超声内镜在腹腔血管疾病的临床应用。其通过多则病例,展示了EUS在这一方面的价值。第1例患者因上消化道出血就诊,反复行胃镜检查均未显示出血灶,EUS检查显示,食管明显曲张静脉,经EUS下曲张静脉内置入血管内钢圈,患者未再发生消化道出血。第二例患者诊断为肝硬化合并胆管梗阻,在接受胆管金属支架置入术后发生胆道出血,原因不明。
EUS检查显示,胆道周围明显静脉曲张,经EUS下曲张静脉内置入血管内钢圈,消化道出血停止。
另外,Michael教授还介绍,在超声引导下穿刺(25 G)门脉分支及肝静脉,并进行压力监测(见下图),对门脉高压患者的治疗很有帮助。
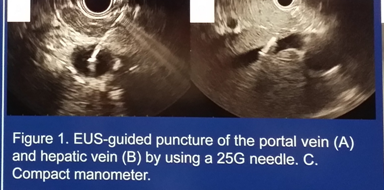
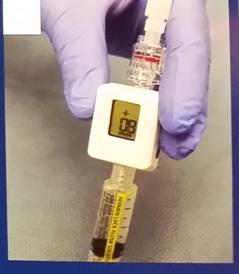
图 超声引导下门脉穿刺、肝静脉穿刺及测压图片
EUS在肿瘤诊治中的作用
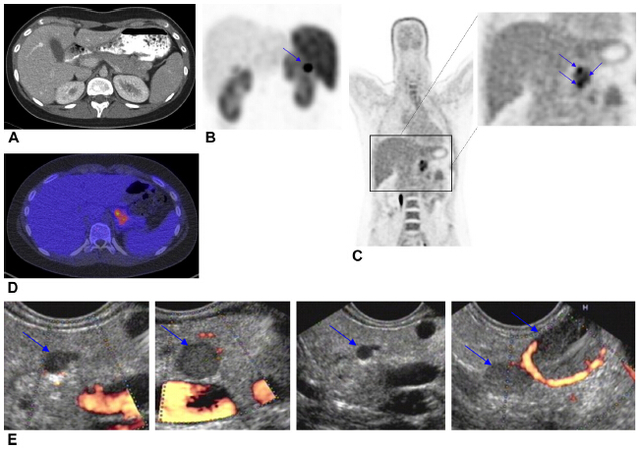
苏哈格(Suhag)博士介绍了EUS对肺癌肾上腺转移的诊断价值。其发现,对于经腹部CT发现的肾上腺异常表现患者,EUS穿刺结果显示,约50%为肺癌转移所致,对于指导患者下一步治疗有很大价值。
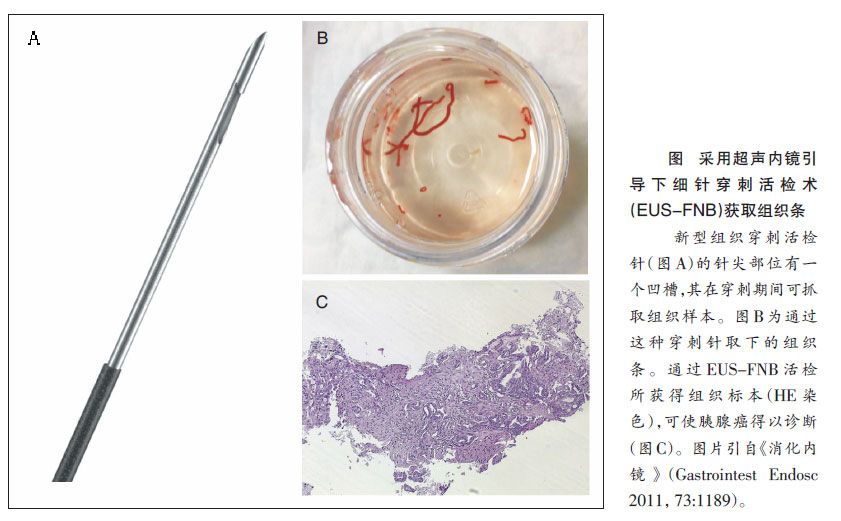
纳维恩(Naveen)博士则报告了消化道肿瘤(主要是胰腺癌)腹腔神经节转移的情况。目前认为,如果EUS检查结果显示腹腔干周围偏低回声结构,穿刺发现肿瘤细胞、同时有神经结构组织而没有淋巴组织,则可认为是肿瘤神经节转移。其研究结果显示,消化道肿瘤(主要是胰腺癌)的腹腔神经节转移率超过10%,但对临床的指导价值目前还不清楚。
EUS与胆管疾病
日本丝井(Itoi)教授向与会者展示了EUS 在胆管穿刺中的应用。EUS胆管穿刺一般用于经内镜逆行性胰胆管造影术(ERCP)不成功或无法进行时。与经皮肝穿胆道引流术(PTCD)相比,EUS成功率与不良反应的发生率无显著差别,且EUS可在ERCP失败后立刻进行,方便安全。另外,Itoi介绍了2则病例,1例患者为肝门胆管癌双塑料支架置入术后发热,考虑胆管炎,再次ERCP困难,EUS检查显示肝内胆管扩张,经肝EUS下穿刺胆管并置入塑料支架后,患者发热症状改善。
另1例为胰腺十二指肠切除术(Whipple)后胆管结石患者,胃内经肝胆管穿刺,造影证实胆总管下段结石,经气囊扩张胆管下端后,结石被推入肠腔。
EUS与胃空肠造瘘
穆昂(Mouen)教授介绍了EUS下胃空肠造瘘的方法。对于胃流出道狭窄且内镜可以通过的患者,可在内镜通过狭窄部位后,在距离胃较近的位置注入美兰与造影剂的混合液体,并在X线监测下,经EUS寻找并穿刺充满液体的肠管;之后,如果回抽可见蓝色液体,则说明穿刺位置正确,可沿穿刺针置入导丝,扩张穿刺通道后,置入造瘘支架。
对于胃流出道狭窄且内镜不能通过(仅导丝可以通过)的患者,则须操作者沿导丝置入扩张球囊至距离胃较近的空肠,并在气囊内注入美兰与造影剂的混合液体,在X线监视下,经EUS寻找并穿刺充满液体的气囊,之后的步骤同“内镜可以通过的胃流出道狭窄患者”。
上述操作需要内镜医生很高的操作技巧,因此,临床应用时应由经验丰富医生操作,并须谨慎选择。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#EUS#
36
#内镜#
24
#DDW#
35
这个厉害
122
的确不错
104
了解
76