Cardiovasc Diabetol:保护2型糖尿病患者的心脏 这种老的降糖药一枝独秀
2018-11-22 吴星 环球医学网
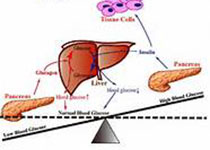
2型糖尿病是心衰发病和发展的独立风险因素。近年来,2型糖尿病患者心衰发病率不断攀升,形势严峻,心脏病的预防和管理成为关注焦点。
2018年,日本学者发表在《Cardiovasc Diabetol》的一项网络Meta分析,考察了口服降糖药物(OADs)对2型糖尿病患者LVM的影响。
研究者对随机对照试验(RCTs)进行网络Meta分析,比较了多种OADs对2型糖尿病患者LVM的影响。
对Medline、Cochrane对照试验注册和ClinicalTrials.gov进行文献检索。研究者纳入评估OADs对2型糖尿病患者LVM影响的RCTs。使用平均标准差(SMD)和95%置信区间(CIs)评估结局。然后,研究者使用随机效应网络Meta分析,比较了OA对LVM的影响。
11项RCTs(1410人)符合入组标准,将这些RCTs纳入到网络Meta分析中。
与安慰剂相比,格列齐特为唯一可显着降低LVM的药物(SMD,-1.09;95% CI,-1.62~-0.57)。当进一步比较各OADs对LVM的影响时,与其他OADs相比(格列本脲、伏格列波糖、二甲双胍、吡格列酮、罗格列酮和西他列汀),仅格列齐特可显着降低LVM。
本研究中,格列齐特是唯一可显着降低2型糖尿病患者LVM的药物。从引发心衰和预防复发的角度考虑时,2型糖尿病患者使用格列齐特可能有诸多获益。
炎症和氧化应激水平的升高,与左心室重构和LVM增加密切相关。格列齐特对氧化应激和炎症的抑制作用似乎是LVM减小的机制。此外,磺脲类受体(SUR)除了在胰腺β细胞表达,还发现心肌细胞表面也表达。格列齐特对胰腺β细胞具有较高的SUR选择性;因此,认为其对心肌细胞中SUR的作用最小。这就是格列齐特与格列本脲相比可显着降低LVM(二者都是磺脲类药物)的原因所在。
Ida S1, Kaneko R2, Murata K2.Effects of oral antidiabetic drugs on left ventricular mass in patients with type 2 diabetes mellitus: a network meta-analysis.Cardiovasc Diabetol. 2018 ;17(1):129. doi: 10.1186/s12933-018-0773-1.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ASC#
40
#DIA#
42
#BET#
38
#降糖药#
32
#2型糖尿病患者#
30
#糖尿病患者#
31
谢谢MedSci提供最新的资讯
53