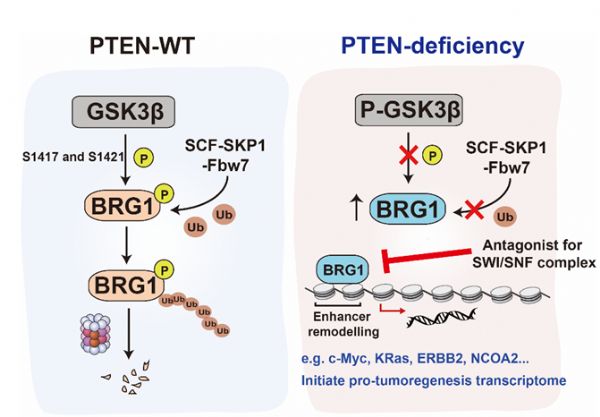
J Clin Invest:研究发现协同致死PTEN缺失前列腺肿瘤的表观遗传基因
2019-01-15 佚名 上海营养与健康研究院
综上所述,该研究阐明了PTEN和BRG1在肿瘤中发挥协同致死作用;靶向BRG1可以作为潜在治疗PTEN缺失前列腺肿瘤的手段。该项研究得到来自科技部国家重点研发计划、国家自然科学基金、中科院等的科研项目资助,同时也得到上海营养与健康院公共技术平台以及动物平台的支持。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#研究发现#
43
#前列腺肿瘤#
56
#EST#
42
学习了,谢谢作者分享!
87
#PTEN#
48
#遗传基因#
51
学习了,谢谢作者分享!
74