FDA授予ADP-A2M4再生医学先进疗法称号,以治疗滑膜肉瘤
2019-12-04 不详 MedSci原创
Adaptimmune Therapeutics 的ADP-A2M4用于治疗滑膜肉瘤,宣布已被授予由美国食品药品监督管理局(FDA)指定的再生医学先进疗法称号(RMAT)。今年早些时候,FDA 授予ADP-A2M4孤儿药称号(ODD),用于治疗软组织肉瘤。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











我是滑膜肉留
20
#滑膜肉瘤#
41
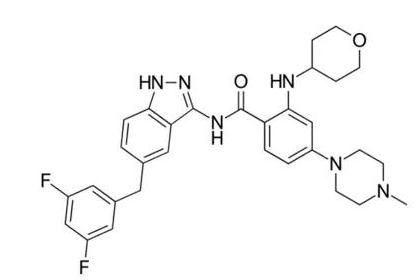
#ADP-A2M4#
28
研究结果令人兴奋
82
研究结果令人兴奋
83
研究结果令人兴奋
95
研究结果令人兴奋
75
研究结果令人兴奋
79
研究结果令人兴奋
17
研究结果令人兴奋
31