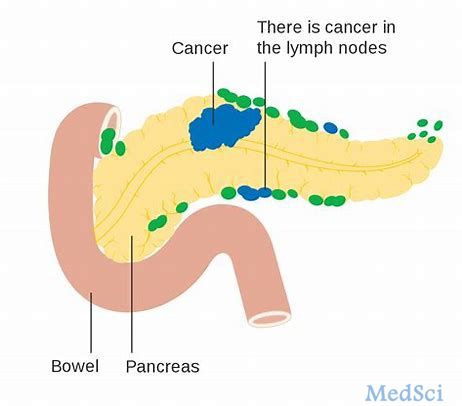
Pamrevlumab治疗局部晚期胰腺癌的III期临床试验正式开始
2019-10-24 Allan MedSci原创
FibroGen近日宣布,Pamrevlumab治疗不可切除的局部晚期胰腺癌(LAPC)的LAPIS III期临床研究中的首位患者已经正式接受治疗。
FibroGen近日宣布,Pamrevlumab治疗不可切除的局部晚期胰腺癌(LAPC)的LAPIS III期临床研究中的首位患者已经正式接受治疗。无法切除的局部晚期胰腺癌患者面临可怕的预后,使用pamrevlumab(一种新型抗纤维化药物)可能会将肿瘤状态从无法切除变为可切除,从而有可能改善患者的预后。
FibroGen临床开发高级副总裁Elias Kouchakji医师表示:“随着LAPIS研究中首位患者的入组,我们很高兴进一步推进pamrevlumab的晚期开发,将其作为局部晚期胰腺癌的治疗方法”。
原始出处:
http://www.firstwordpharma.com/node/1675716#axzz63E8SwRis
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#II期临床试验#
24
#MRE#
34
#局部晚期#
44
#mAb#
0
#I期临床试验#
33
#III#
18
#pamrevlumab#
36
#I期临床#
27
#局部晚期胰腺癌#
25
#晚期胰腺癌#
36