J AM COLL SURGEONS:乳房重建术后,使用抗生素24小时足矣
2016-03-31 MedSci MedSci原创
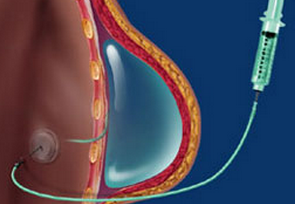
新的研究发现快速组织扩张乳房重建术后,使用抗生素24小时预防感染与更长时间的效果相当,并且不增加额外的感染并发症,研究发表在于3月3日 Journal of the American College of Surgeons.
新的研究发现快速组织扩张乳房重建术后,使用抗生素24小时预防感染与更长时间的效果相当,并且不增加额外的感染并发症,研究发表在于3月3日 Journal of the American College of Surgeons.
CDC现有的指南也推荐在TE-IBR后只使用24小时,但临床实践却不是这样。主要作者Brett T. Phillips医生来自北卡罗来纳州达勒姆杜克大学医学院,他和同事对112个TE-IBR病人进行了一项前瞻性非劣效性试验(180个乳房)。62个病人使用24小时抗生素后停止,50个病人使用抗生素直到引流管移除。
所有受试者都在术前根据体重指数(低于或高于30)使用1-2g 头孢唑林或若阿司匹林过敏则使用600-900mg的克林霉素。如果有必要的话,术中抗生素是在初次用药4-6小时后给予。所有受试者都接受了24小时的静脉注射,持续口服抗生素的给予500mg头孢氨苄,1天4次,或300mg的克林霉素1天3次。
24小时治疗组有12人发生手术部位感染,延长治疗组有11人(19.4% vs 22.0%)。延长治疗组有7人需要静脉抗生素,整体的植入物滑落有7人(14.0%)。24小时治疗组有4个病人需静脉抗生素,3个病人需重新植入假体(4.8%)。糖尿病病人,术后皮下血肿,或伤口裂开的病人更可能发生术后感染(P<0.02)。
作者提到了此实验的几点局限,包括他们的非劣效性研究设计妨碍了证明24小时治疗组的优势作用,由于经济和逻辑限制,缺乏安慰剂和双盲。
原始出处:
Brett T. Phillips, MD, Mitchell S. Fourman,et al,Are Prophylactic Postoperative Antibiotics Necessary for Immediate Breast Reconstruction? Results of a Prospective Randomized Clinical Trial,,J Am Coll Surg March 30, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







不错哦,会学到很多
0
#24小时#
33
#Coll#
37
xuexike
136