高渗性非酮症糖尿病脑病二例
2019-06-18 刘秀丽 张戟风 许美 临床放射学杂志
例1女,60岁。糖尿病20年,口服降糖药,血糖控制理想。因受凉感冒,发热4天,突发昏迷入院,CT检查示:双基底节豆状核区对称高密度影,边界清晰(图1A)。MRI扫描:扩散加权成像(DWI)双基底节豆状核区对称性低信号(图1B),T1WI双侧基底节豆状核区对称高信号(图1C),MRIT2WI豆状核呈等信号(图1D)。血糖34.1mmol/L,尿糖(++++),尿酮体(-),尿素氮25mmol/L,肌
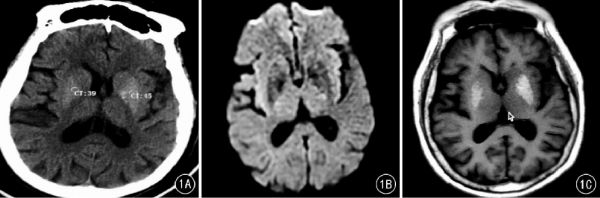
例1女,60岁。糖尿病20年,口服降糖药,血糖控制理想。因受凉感冒,发热4天,突发昏迷入院,CT检查示:双基底节豆状核区对称高密度影,边界清晰(图1A)。MRI扫描:扩散加权成像(DWI)双基底节豆状核区对称性低信号(图1B),T1WI双侧基底节豆状核区对称高信号(图1C),MRIT2WI豆状核呈等信号(图1D)。血糖34.1mmol/L,尿糖(++++),尿酮体(-),尿素氮25mmol/L,肌酐403mmol/L,BUN/Cr比值35∶1。诊断:高渗性非酮症糖尿病脑病。经临床对症治疗后,患者意识清晰,活动自如,血糖12.37mmol/L,尿糖(+),尿酮体(-),其余化验指标大致恢复正常。20天后复查CT平扫显示:双基底节豆状核区高密度影消失,呈等密度改变(图1E)。
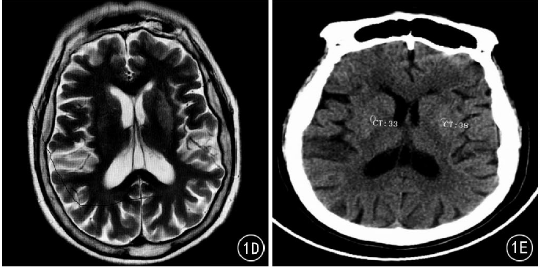
图1A~E例1。A.CT横断扫描显示:双基底节豆状核区对称性高密度影,边界清晰。B.MRI扫描显示:DWI双基底节豆状核区对称性低信号。C.MRI扫描:T1WI双侧基底节豆状核区对称高信号。D.MRI扫描:T2WI豆状核呈等信号。E.20天后复查CT显示:双基底节豆状核区高密度影消失,呈等密度改变
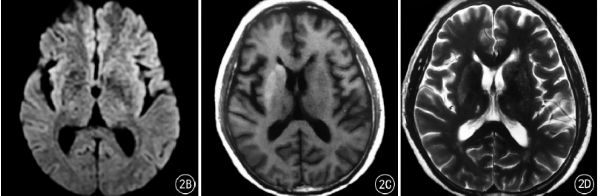
例2男,70岁。糖尿病25年,胰岛素控制血糖5.6~7.1mmol/L。左股骨颈骨折后卧床2天,突发意识障碍入院,CT检查示:右基底节尾状核、豆状核区高密度影,边界清晰(图2A)。MRI检查显示:DWI双基底节豆状核区对称性低信号(图2B)。T1WI右基底节尾状核、豆状核区高信号(图2C),MRIT2WI右基底节尾状核、豆状核区等信号(图2D)。血糖35.4mmol/L,尿糖(++++),尿酮体(-),尿素氮23mmol/L,肌酐488mmol/L。诊断为:高渗性非酮症糖尿病脑病。经临床对症治疗后,患者意识恢复,血糖10.1mmol/L,尿糖(+),尿酮体(-)。复查CT平扫显示:右基底节尾状核、豆状核区高密度影消失。
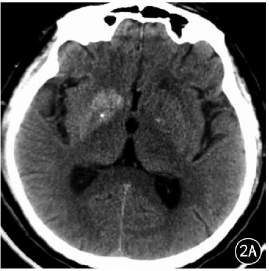
图2A~D例2。A.CT横断面扫描示:右基底节尾状核、豆状核区高密度影,边界清晰。B.MRI检查显示:DWI双基底节豆状核区对称性低信号,右侧明显。C.MRI扫描T1WI右基底节尾状核、豆状核区高信号。D.MRI扫描T2WI右基底节尾状核、豆状核区等信号
讨论
高渗性非酮症糖尿病脑病也称为高渗性非酮症性昏迷(hyperosmolar non-ketotic diabetic coma,HNDC),是应激状态下发生的血糖迅速升高导致的急性神经系统异常和意识障碍综合征。典型临床特点包括:高血糖、高血浆渗透压,意识进行性丧失和缺乏明显酮症,严重时昏迷。临床诊断标准包括:血糖≥33mmol/L(600mg/dl):血浆有效渗透压≥320mmol/L:血清HCO3≥15mmol/L或动脉血气检查示pH值≥7.30:尿糖强阳性,尿酮体阴性或弱阳性。以上前3项可作为必要诊断依据,第4项根据临床情况不同可有变化。
HNDC患者发病时,血糖急骤上升,严重糖代谢紊乱,导致细胞外液呈高渗状态,细胞发生低血容量高渗性脱水,大脑皮质供血不足和缺氧,临床出现精神神经症状,甚至昏迷。临床常见诱因包括:应激和感染、严重脱水或摄水不足、肾衰竭、高糖摄入及大量使用糖皮质激素、利尿药、硫唑嘌呤及其他免疫抑制剂等。HNDC好发于糖尿病患者,非糖尿病患者也可发生。
既往文献多以临床报道为主,鲜有影像学报道,随着影像学检查在临床工作中的广泛应用,对于意识障碍患者,特别是突发昏迷患者,首选急诊CT检查除外脑血管病,显示双基底节豆状核区出现对称或非对称性可逆性高密度影,应该想到HNDC可能,特别是对中老年患者有常见诱因,应立即配合实验室检查。对于影像学表现的病理学基础有各种说法,主要包括微出血、脑缺血、不知名物质沉积等。CT表现为基底节区高密度可能是微出血,国外有病灶区存在含铁血黄素沉积的尸检报道,但是MRI显示T1WI高信号、T2WI呈稍低信号或等信号,与常规血肿演变过程不同,本组2例患者复查CT显示病灶周围没有水肿带,无明显占位效应,吸收、消散迅速,病灶完全吸收,无明显软化灶形成,确实与常见血肿演化过程不同。
也有研究者认为基底节区星形胶质细胞胞质内蛋白水化层使T1弛豫时间缩短,T1WI呈高信号脑缺血改变,DWI呈异常低信号不符合缺血改变。正电子发射计算机断层显像(PET)检查发现基底节区的血流灌注及糖的代谢显著降低,支持缺血改变,这一观点与脑缺血在CT检查时表现为低密度改变相悖。还有学者认为是可逆性钙盐沉积或钙内流形成CT高密度影,脑缺血后的星形胶质细胞内锰沉积形成T1WI高信号改变。
鉴别诊断:包括肝性脑病及糖尿病脑血管病。肝性脑病MRI表现可见双基底节区对称性T1WI高信号改变,但CT表现为等密度改变。糖尿病造成血管内皮损害,血小板聚集及血液黏稠度增加,造成血管狭窄、阻塞,脑组织缺血缺氧,脑血管病发生率很高,其中88%是脑梗死。脑梗死急性期DWI呈高信号改变,CT呈低密度改变。虽然HNDC的影像学表现原理不是很清楚,根据CT、MRI等特征性影像学表现,结合实验室检查及临床表现可以诊断该病。
原始出处:
刘秀丽,张戟风,许美,刘景旺,刘颖.高渗性非酮症糖尿病脑病二例[J].临床放射学杂志,2018(03):523-524.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#非酮症#
40
#高渗性#
39
#脑病#
26
#酮症#
41
谢谢MedSci提供最新的资讯
56