Heart:急性冠状动脉综合征后停止双重抗血小板治疗与心血管事件
2018-07-22 xing.T MedSci原创
由此可见,与ACS患者DAPT停药后晚期相比,DAPT停药后早期心血管事件发生率没有显著增加。年龄较大、DAPT持续时间较长和未进行血运重建治疗与DAPT停止后长期随访期间心血管事件风险增加有关。
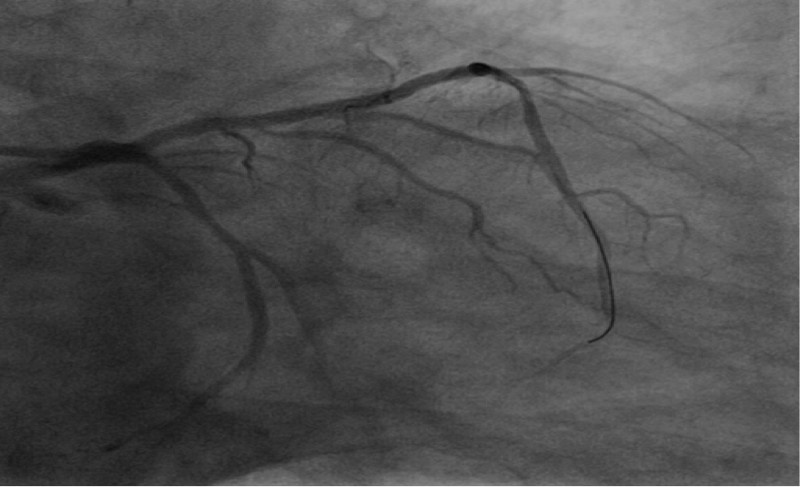
近日,心脏病领域权威杂志Heart上发表了一篇研究文章,该研究旨在评估急性冠状动脉综合征(ACS)后停止双重抗血小板治疗(DAPT)后心血管事件是否增加,并探讨长期随访期间DAPT停止后复发事件的预测因素。
研究人员进行了一项回顾性观察性队列研究。研究人员纳入了连续就诊的ACS患者,他们于2008年1月至2013年12月期间从苏格兰医院出院,并在出院后接受DAPT,然后接受抗血小板单药治疗。在DAPT治疗的每个90天期间和停止DAPT后的90天期间评估心血管事件的发生率。心血管事件被定义为死亡、ACS、短暂性脑缺血发作或卒中的复合事件。 Cox回归用于确定DAPT停止后心血管事件的预测因子。
该研究纳入了1340例患者(男性占62%,平均年龄为64.9±13.0岁)。在DAPT期间(平均DAPT持续时间为175.1(155.3)天),心血管事件发生率为15.7%(n=211),DAPT停止后(平均随访时间为2.7年)为16.7%(n=188)。DAPT停止后心血管事件的独立预测因素包括年龄(HR为1.07; 95%CI为1.05-1.08; p<0.001)、DAPT持续时间(HR为0.997; 95%CI为0.995-0.998; p<0.001)并且在此期间进行血运重建治疗(HR为0.58; 95%CI为0.39-0.85; p=0.005)。
由此可见,与ACS患者DAPT停药后晚期相比,DAPT停药后早期心血管事件发生率没有显著增加。年龄较大、DAPT持续时间较长和未进行血运重建治疗与DAPT停止后长期随访期间心血管事件风险增加有关。
原始出处:
Wardati Mazlan-Kepli,et al. Cessation of dual antiplatelet therapy and cardiovascular events following acute coronary syndrome. Heart. 2018. http://dx.doi.org/10.1136/heartjnl-2018-313148
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#冠状动脉综合征#
32
#血管事件#
32
学习了
50
好文章学习了
63
学习
50
#ART#
31
#双重抗血小板治疗#
37
#综合征#
29
#HEART#
34
好
64