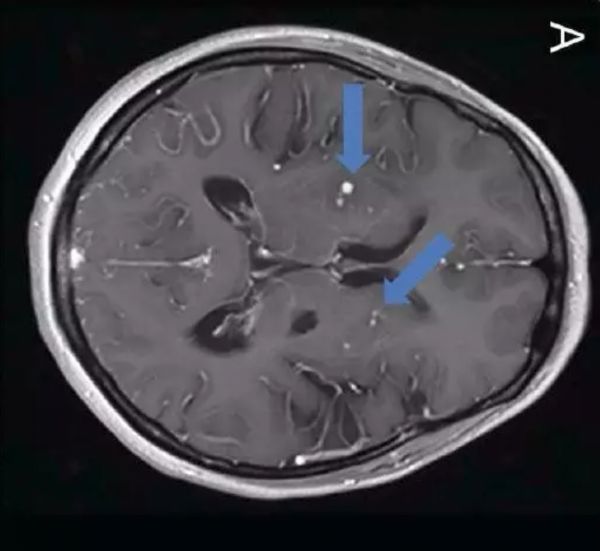
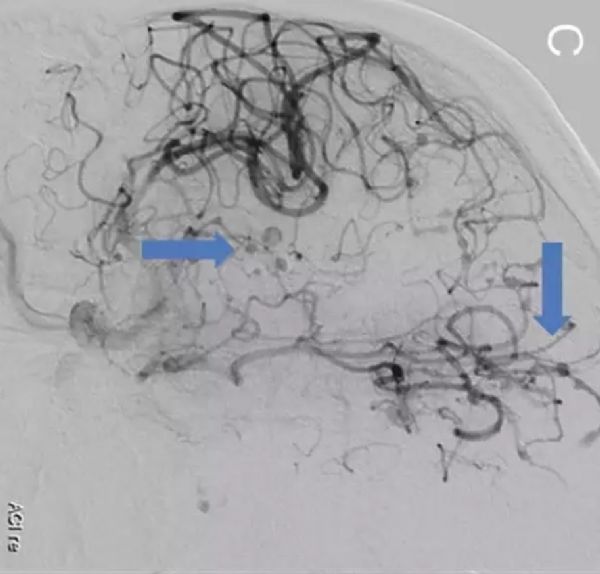
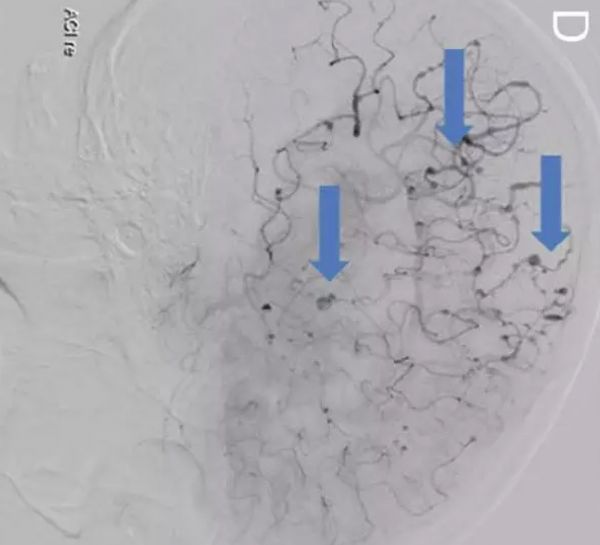
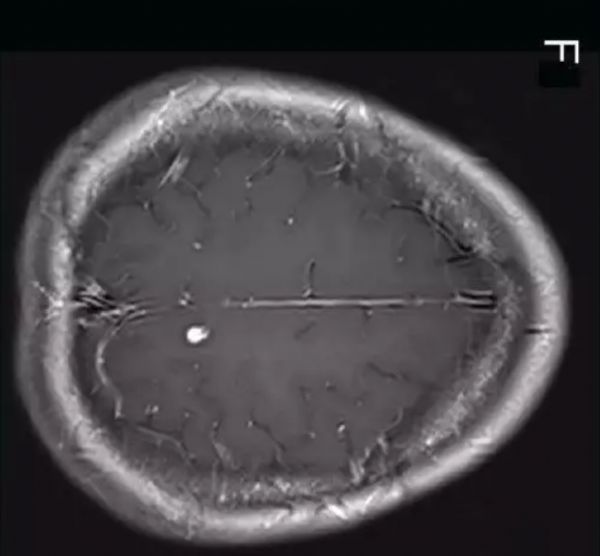
Neurology:HIV相关脑血管病伴随多发动脉瘤一例
2017-10-07 杨中华 脑血管病及重症文献导读
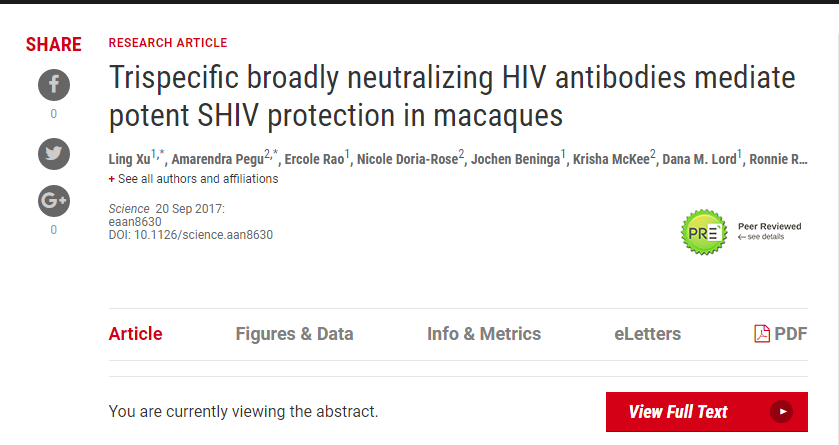
在儿童,HIV相关脑血管病伴随多发动脉瘤已经被广泛报道。对于成人HIV患者,如果脑脊液中病毒负荷量较高,也应该考虑与HIV有关。典型影像学表现为结节和梭型动脉瘤,其病因可能与自身免疫有关,容易和结节性多动脉炎混淆。这些动脉瘤可以引起蛛网膜下腔出血,也可以由于血栓形成导致脑梗死。高效抗逆转录病毒疗法是有效的。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血管病#
30
#Neurol#
35
#多发动脉瘤#
38
学习了
84
学习了.谢谢
68
谢谢.学习了
80
学习了受益匪浅
72
学习了.涨知识
82
henhao
21
好好努力学习
27