Eur Urol:重点治疗后机器人辅助的根治性前列腺切除术的效果研究
2019-04-09 AlexYang MedSci原创
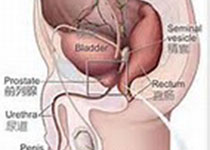
那些经历重点治疗(FT)后的前列腺癌(PC)局部复发患者,进行根治性前列腺切除术(RP)后的结果和毒性情况的相关研究很少。最近,有研究人员对进行抢救性机器人协助RP(S-RALP)的患者的围手术期,肿瘤和功能结果情况进行了鉴定,并确定了S-RALP失败的风险因素。研究是一个多中心的群体研究,包括了82名在FT后经历S-RALP的患者。所有的参与者均具有组织学确定的PC复发。研究发现,无进展生存在术
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#前列腺切除#
34
#切除术#
33
#机器人#
29
#机器人辅助#
27
#机器#
29
#根治#
30
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
43