颜红兵教授:及时再灌注,须分秒必争!
2018-06-12 佚名 医学界心血管频道
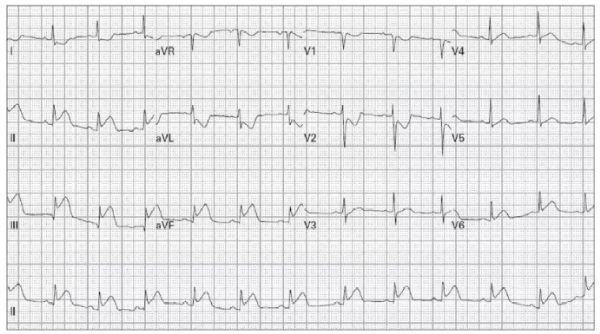
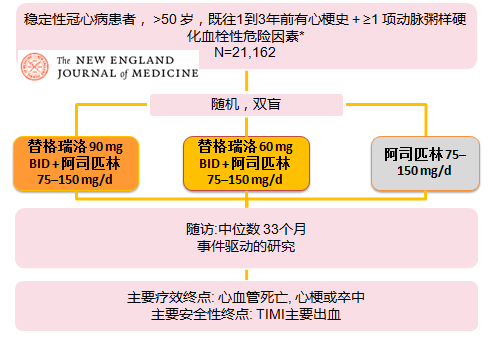
前不久,《ST段抬高型急性心肌梗死院前溶栓治疗中国专家共识》(以下简称《共识》)正式发布,旨在帮助院前医疗急救人员对ST段抬高型急性心肌梗死(STEMI0患者的治疗策略做出选择。中国医学科学院阜外医院的颜红兵教授作为该《共识》的编撰专家之一,在接受采访时,就我国目前STEMI诊疗现状和院前溶栓的热点问题分享了自己的观点。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










谢谢分享.学习了
82
recanolization
69
阅
77
了解了解.继续关注
66
好文献学习了
78
学习学习再学习
27