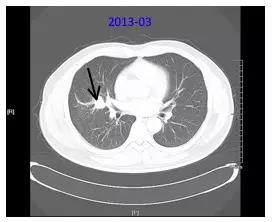
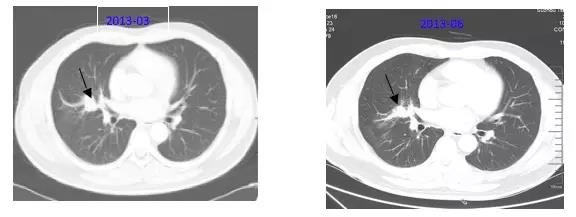
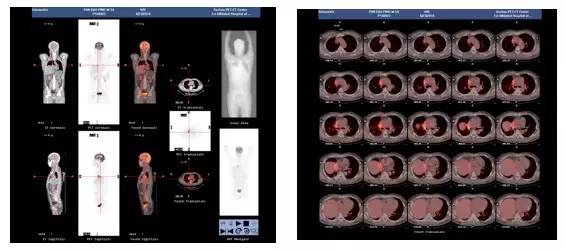
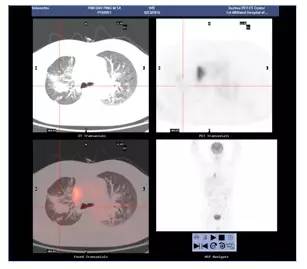
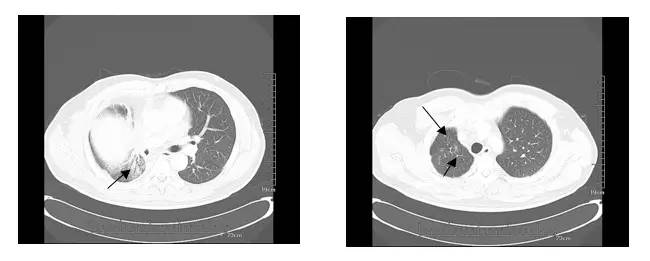
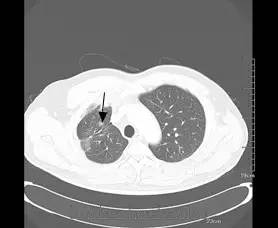
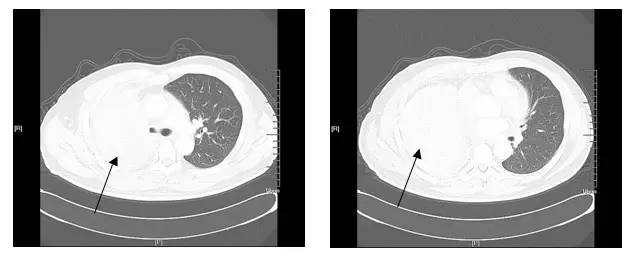
病例讨论:结肠癌肺转移MDT诊疗
2017-08-17 张宛莉,熊峰,赵荣昌,朱春荣 苏州大学附属第一医院肿瘤内科
一般情况:KPS评分90分,有吸烟史20+年,不规律饮酒史20+年,无高血压、糖尿病、冠心病、慢支等病史

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#病例讨论#
44
涨知识了多谢分享
74
学习了谢谢分享!!
73
#MDT#
32
#肺转移#
43
谢谢分享
67
学习了谢谢分享
61