2017AHA/ASA关于"无症状脑血管病"的科学声明
2018-04-17 脑血管病及重症文献导读 杨中华
2017年2月AHA联合ASA共同在Stroke上发布了无症状脑血管病的卒中预防科学声明,现将推荐意见摘录如下。
2017年2月AHA联合ASA共同在Stroke上发布了无症状脑血管病的卒中预防科学声明,现将推荐意见摘录如下。
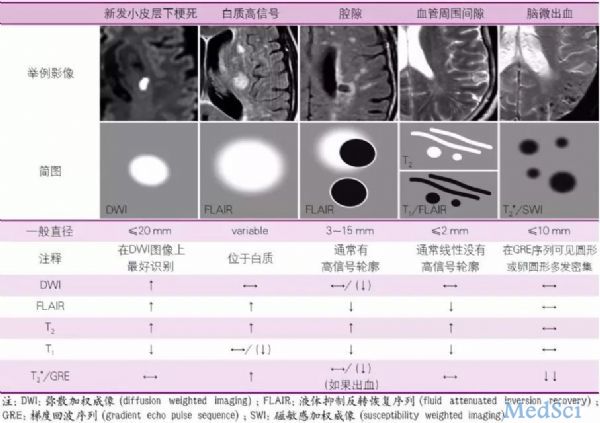
无症状脑血管病(Silent Cerebrovascular Disease)主要表现包括:新发小皮层下梗死(recent small subcortical infarcts)、血管源性腔隙(lacunes of presumed vascular origin)、血管源性白质高信号(white matter hyperintensities of presumed vascular origin)、血管周围间隙(perivascular spaces,PVS)和脑微出血(cerebral microbleeds)。
影像学诊断
MRI诊断无症状脑血管病比CT更加敏感
影像学报告应该按照STRIVE标准描述无症状脑血管病
应该采用视觉等级量表描述血管源性白质高信号,比如MRI Fazekas量表
无症状脑血管病的检查
评价常见血管病危险因素,根据脉搏判断有无房颤
无症状脑梗死应该进行同侧颈动脉影像学检查
栓塞样无症状梗死应该进行超声心动图检查
体积较大(> 1cm)无症状出血者应该进行无创CTA或MRA检查
无症状梗死患者的卒中预防
仔细询问病史,判断是否为症状性脑梗死
按照AHA/ASA缺血性卒中一级预防指南预防卒中
这种情况下阿司匹林预防卒中的作用尚未被研究
临床医生应该意识到这将增加未来卒中的风险,当制定某些治疗决策时应该参考这些信息,比如房颤抗凝、颈动脉狭窄血运重建、治疗高血压以及开始他汀治疗时。不过,临床医生还应该意识到无症状脑梗死对治疗决策所起到的作用尚未被RCT研究证实。
血管源性白质高信号(WMH)患者的卒中预防
按照AHA/ASA缺血性卒中一级预防指南预防卒中
在缺乏其他危险因素的情况下,仅仅WMH是否可以作为使用阿司匹林理由尚不清楚
临床医生应该意识到这将增加未来卒中的风险,当制定某些治疗决策时应该参考这些信息,比如房颤抗凝、颈动脉狭窄血运重建、治疗高血压以及开始他汀治疗时。不过,临床医生还应该意识到WMH负荷对治疗决策所起到的作用尚未被RCT研究证实。
无症状微出血的抗凝和其他治疗
具有抗凝指证的脑微出血患者给予抗凝治疗是合理的
当需要抗凝治疗时,新型口服抗凝剂优于华法林
经皮左心耳封堵术可以作为抗凝治疗的替代方案
具有抗血小板指证的脑微出血患者给予抗血小板治疗是合理的
抗栓治疗前不需要MRI筛查微出血
无症状微出血会同时增加将来缺血性卒中和脑出血的风险
按照AHA/ASA缺血性卒中一级预防指南预防卒中
按照AHA/ASA指南推荐意见预防脑出血
无症状微出血患者急性缺血性卒中治疗的安全性
合并微出血的急性缺血性卒中患者,有指证者可以静脉给予阿替普酶治疗
合并微出血的急性缺血性卒中患者,有指证者可以进行血管内血栓切除术
合并微出血的急性缺血性卒中患者,绕过静脉阿替普酶而直接血管内血栓切除术的作用尚未被证实
人群筛查
根据当前证据,不应对无症状普通人群进行MRI筛查无症状脑血管病
注:最重要的一句话无症状脑血管病应该“按照AHA/ASA缺血性卒中一级预防指南预防卒中”。
下表引自王拥军教授《顿悟》:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ASA#
37
#血管病#
25
学习了.谢谢作者分享!
61
#AHA#
25
#无症状#
36