【一般资料】
患者,男,62岁
【主诉】
因发现左臀部肿物30余年于2017年8月19日入院。
【体格检查】
左臀部较对侧明显膨隆,左臀部下方可见一斜行长约10CM的瘢痕,无红肿及窦道形成,局部皮肤正常,皮温略高,可触及一大小约18CM×30CM×13CM的囊实性肿物,表面质软,无压痛,活动度可,髋关节活动正常。
【辅助检查】
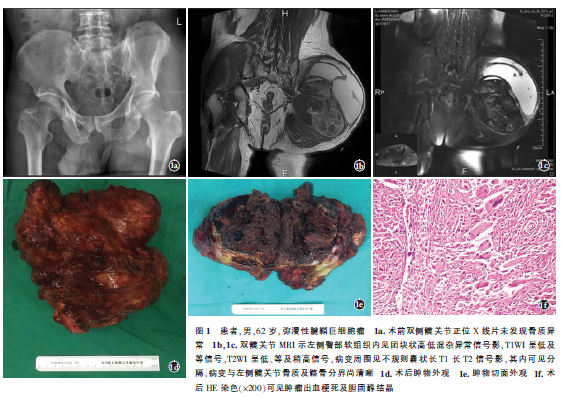
术前骨盆X线片(图1a)未报明显骨质异常。臀部彩超:可见囊性包块,其内可见少量分隔,探头挤压可见细弱光电波动,其周边可见1个15CM×13CM×14CM的实性包块,其内未见明显血流,提示左臀部混合型占位。双髋关节MRI(图1b,1c)示左侧臀部软组织内见团块状高低混杂异常信号影,与臀大肌关系密切,大小约13.4CM×8.7CM×14.9CM,T1WI呈低及稍高信号,T2WI呈低、等及稍高信号,病变周围见不规则囊状长T1、T2信号影,其内可见分隔,病变与左侧髋关节骨质及髂骨分界尚清晰。患者入院后行常规检查、男性肿瘤标志物及全身骨显像检查,检查结果无明显异常。
【既往史】
患者40年前左臀部利器刺伤史,于当地医院手术治疗(具体不详),自述清创缝合后愈合良好,术后无感染、红肿及窦道形成。
【治疗】
患者入院后第2天行B超引导下左臀部穿刺置管术,引出暗红色血性液体约1500ml,取穿刺液送检,穿刺液血培养、结核菌涂片及一般细菌真菌培养均未有明显异常。入院后第3天局麻下行左髂动脉造影示左侧髂内动脉显著增粗,分支增多、紊乱,且血管分支受肿物挤压呈包绕征象,左侧臀上臀下动脉为主要病变供血血管,遂行左臀上下动脉血管栓塞术。入院后第4天患者在全麻下行左臀部肿瘤扩大切除术。全麻生效后,沿原穿刺管引出暗红色血性液体约1800ml,此时可触及左臀部实性肿物,取左臀部弧形切口,逐层广泛分离皮肤、皮下脂肪、浅筋膜至臀大肌,术中见臀大肌纤维挛缩变薄,探查肿物位于臀大肌深面,不规则团块状,大小约13CM×7CM×15CM。肿物底部邻近坐骨神经,包膜完整,可见肿物分叶,有囊腔分隔,因肿物巨大,逐层切开肿物包膜,包膜内可见大量铁锈色液体及坏死组织,质韧图(1e)。分离保护坐骨神经后将肿物广范围游离解剖和去除其肿物下界深达坐骨大切迹,术中完整切除肿物(图1d),用碘伏和生理盐水反复冲洗,逐层缝合,留置引流管。术后将肿物送检病理。术后病理回报:结节样肿物1枚,体积14CM×14CM×10CM,表面不光滑,切面弥漫出血、坏死样,周边见1个破裂囊腔,直径约12CM,内壁淡褐色,尚光滑,未见内容。HE染色:肿瘤组织内可见肿瘤出血梗死及胆固醇结晶(图1f)。免疫组化:ki-67(<10%)。病理诊断为腱鞘巨细胞瘤(弥漫型)。术后患者恢复良好,术后3个月随访见左臀部肿物切口愈合良好,肿物无复发,无感觉及运动功能障碍。
【讨论】
腱鞘巨细胞瘤可以分为局限型腱鞘巨细胞瘤和弥漫型腱鞘巨细胞瘤(D-TGCT)两种类型。按生长部位又可以分为关节内型和关节外型,关节内型弥漫腱鞘巨细胞瘤又称为色素沉着绒毛结节性滑膜炎(PVNS);关节外型是一个缓慢增长且拥有很好预后的病变,通常可以完整切除。该肿瘤是局部侵袭性的,良性的,33%~50%会复发,但是多发转移到其他器官比较罕见。D-TGCT病因不明,常见于20~50岁,女性多于男性。起源于腱鞘及滑囊的滑膜细胞,是滑膜样单个核细胞破坏样增生,组织学特性与色素沉着绒毛结节性滑膜炎相同,表现为沿肌腱向关节外生长,并累及小区域滑膜,缺乏清晰边界,呈膨胀性和浸润性生长。术前诊断困难,临床及影像学检查缺乏特异性。D-TGCT主要累及膝、踝、髋等负重关节,肌内型肿瘤国内外仅报道了几例。肌内型肿瘤可以影响任何肌肉,但大多数位于下肢,包括臀部、大腿和小腿,这与本例情况相一致。而Yun等报道了1例上肢三角肌内的DTGCT。尽管肌内D-TGCT很少见,但重要的是要知道它们可以渗透到周围软组织并具有高复发率,需要完全手术切除和定期随访。(1)鉴别诊断。PVNS:好发于膝、髋等关节,主要表现为关节肿胀和轻微疼痛,关节活动轻度受限。局部检查可触及肿胀的关节,有压痛。关节穿刺可抽出血性或棕褐色液体。X线平片可见病变关节弥漫性或局限性肿胀,周围可见结节阴影,后期关节间隙变窄,病变多弥漫,累及关节内外组织,与周围组织分界不清,难以手术完整切除。但本例病变孤立存在于臀大肌内,瘤体巨大,且未与关节腔相通,无骨质受累,与周围组织分界尚清,根据病变形态、位置特点以资鉴别。滑膜肉瘤:好发于四肢,多见于大关节,也可发生于肌腱和筋膜上。滑膜肉瘤生长迅速,具有恶性肿瘤特点。早期通常表现为深部无痛性肿物,后期肿瘤逐渐增大可出现疼痛。其X线或CT有价值的影像学改变是肿瘤邻近骨质可有骨质破坏、受压骨吸收等改变,表现为邻近关节的不规则、结节状软组织肿块,病灶内可有钙化或骨化。由于肿瘤内出血,通常在T2WI具有不均匀的信号强度,这点容易与本病相混淆,但滑膜肉瘤特征性MRI表现为团块内多可见液-液水平及软组织钙化。本例X线平片及核磁多表现为软组织肿块,无钙化表现。结合病史、临床表现及影像学特点可与本病鉴别。肌间血管瘤:骨骼肌间血管瘤是指原发于骨骼肌的血管瘤。呈浸润性生长,常局限于单块肌肉,部分患者以肿块伴有疼痛为主诉表现,最常见于四肢及躯干。其病灶位置深,侵袭范围广,临床特征不易观察。影像学检查对本病诊断意义较大,彩色超声检查可见典型肌间血管瘤内部常有蜂窝样结构或混合型回声,MRI敏感性更高,可清晰显示肿物大小和范围。本例患者超声及血管造影提示肿块血流丰富,故容易误诊为血管瘤。而本例患者病变处血流丰富可能与肿块本身伴随出血、坏死有关。结合肿物病变位置、形态特点及影像学特点与本例病变鉴别有一定难度,以病理结果为准。(2)治疗方案的选择。D-GCTS属于局部侵袭性较弱的非转移性肿瘤,大多是生长缓慢、无痛的良性肿瘤,目前首选的治疗方法是手术切除,以期最大限度保留肢体功能。本例患者虽瘤体巨大,但边界尚清,且全身骨显像及肺部CT排除肿瘤远处转移可能,故Ⅰ期行左臀部肿瘤扩大切除术。肿物及切缘均送检病理,术中快速病理排除了恶性肿瘤的诊断。目前对于软组织肉瘤应该采用的阴性切缘并没有严格的定义,但有关资料表明对于局限侵袭性较弱的低度恶性肿瘤,肿瘤外>1CM的阴性手术切缘或切缘含有完整的深筋膜均可达到根治效果,可以不进行术后放疗。另一项报告表明,肌内型复发率低于其他类型,因为肌内肿物较累及关节的肿物更容易完全切除。腱鞘巨细胞瘤的化学及生物学治疗效果尚不明确,缺乏临床大样本的随访数据支持。局部放疗多针对弥漫性生长的侵袭性D-GCTS、手术无法完整切除、肿瘤累及范围较广切除后有可能复发或切除后复发的患者。本例术中未见明确恶性表现,臀部肿物得到完整切除,切缘>1CM,遂术后未辅以放疗。但由于肌内型D-TGCT比较罕见,远期临床结果仍然不清楚,有赖于进一步随访观察。综上所述,D-TGCT病因不明,主要累及膝、踝、髋等负重关节,鲜有单纯累及肌肉的报道。单纯累及臀大肌部位的D-TGCT,单基于影像学检查的诊断具有挑战性,其诊断主要依赖病理学检查。本病例采用左臀部肿瘤扩大切除术,考虑肿瘤局部侵袭性较弱,术后未予进一步处理。患者术后3个月来院复查未发现肿瘤复发的情况。
原始出处:
陈龙,吕龙龙,吕浩,黄琦,徐声鸣,牛丰.臀大肌弥漫型腱鞘巨细胞瘤1例[J].中国骨伤,2018,31(04):373-375.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#腱鞘巨细胞瘤#
38
学习了.谢谢分享
46
#细胞瘤#
18
#巨细胞#
18
学习了受益匪浅
57