Blood:红细胞铁蛋白缺乏会导致血清铁不足,并促进氧化应激导致的溶血
2018-09-14 MedSci MedSci原创
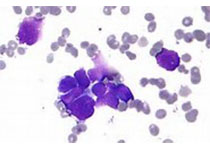
中心点:红细胞上的FPN对血液的铁含量至关重要。FPN缺陷易导致红细胞氧化损伤。摘要:铁蛋白(FPN),是目前唯一已知的脊柱动物的铁出口,将铁从肠道、脾和肝血细胞转运至血液,为机体的其他组织和细胞提供铁。大部分循环铁被红细胞用来合成血红蛋白。De-Liang Zhang等人发现红细胞不仅会消耗大部分的铁,还可向血液返回大量的铁。特异性敲除有核红细胞Fpn的小鼠(Fpn KO)表现为血清铁水平低、组
红细胞上的FPN对血液的铁含量至关重要。
FPN缺陷易导致红细胞氧化损伤。
摘要:
De-Liang Zhang等人发现红细胞不仅会消耗大部分的铁,还可向血液返回大量的铁。特异性敲除有核红细胞Fpn的小鼠(Fpn KO)表现为血清铁水平低、组织铁过负荷,脾肝FPN表达量增加,但无铁调素水平改变。研究人员还发现有中度溶血性贫血的Fpn KO小鼠对苯肼诱导的氧化应激敏感,但暴露于低铁饮食和放血时,可耐受铁缺乏,提示Fpn KO小鼠的贫血是由红细胞铁过负荷和氧化损伤导致的,而不是RBC生成缺陷。
此外,研究人员还发现携带功能获得性FPN突变的患者的平均红细胞容积(MCV)评估与血清铁蛋白饱和度正相关,但功能丧失性FPN突变患者的MCVs无此现象,提示有核红细胞是通过FPN将铁转运至血液。
总而言之,本研究表明红细胞的FPN在维持系统铁稳态和保护RBCs免受氧化损伤过程中发挥至关重要的作用,加深了我们对FPN疾病的病理生理的了解。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血清铁#
40
#红细胞#
38
#应激#
39
嗯嗯,学习学习。
78
学习了谢谢
71
学习了
74