RVAS(低频突变关联分析)成为研究新宠,超越GWAS
2016-01-24 梁忱 诺禾致源
聊聊一个渐渐火热起来的疾病研究新方法:RVAS(低频突变关联分析)。展望之前,我们先来温习一下,啥叫GWAS。 辩证地看待GWAS 复杂疾病遗传学研究中有个神奇的名词:GWAS。就在刚刚过去的十年里,GWAS是这个星球上最热门的复杂疾病分析方法。从不知所云的MoyaMoya病到我们看得见、摸不透的身高、体重、甚至性格,都被GWAS研究了个遍。 图1 全基因组关联分析(
聊聊一个渐渐火热起来的疾病研究新方法:RVAS(低频突变关联分析)。展望之前,我们先来温习一下,啥叫GWAS。
辩证地看待GWAS
复杂疾病遗传学研究中有个神奇的名词:GWAS。就在刚刚过去的十年里,GWAS是这个星球上最热门的复杂疾病分析方法。从不知所云的MoyaMoya病到我们看得见、摸不透的身高、体重、甚至性格,都被GWAS研究了个遍。
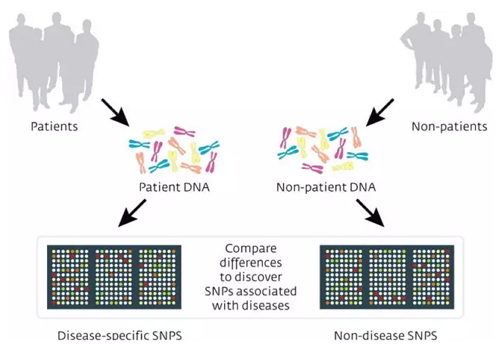
图1 全基因组关联分析(GWAS)(来自Pasieka Science Photo Library)
GWAS,是全基因组关联分析(Genome-wide association study),运用统计学计算来搜寻在患者人群和正常人群中的分布有显著差异的疾病关联变异位点的方法。虽然分析中需要考虑各类复杂的影响因素,但它的原理就是这么简单。
不过如果细究起来,GWAS应该分为两个截然不同的分析项目:基于常见突变的关联分析(Common variant association study, CVAS)和基于低频突变的关联分析(Rare variant association study, RVAS)。
曾经,基于芯片的常见突变关联分析CVAS锋芒毕露。但随着疾病研究的深入,从前人们视为畏途的低频突变关联分析RVAS在高通量测序时代已渐渐成为大家瞩目的焦点。

CVAS的梦想与现实
从本世纪初起,科学家们就有一个梦想:基于『常见疾病 – 常见突变』的假设,人们希望通过常见突变的解析,找到所有像高血压、糖尿病、精神分裂症等与健康息息相关的常见疾病的遗传学基础。
常见突变关联分析(CVAS)基于MAF > 5%的SNP位点,可以由SNP分型芯片或低深度测序来完成。从2005年左右开始,常见突变关联分析(CVAS)为人类的数百种复杂疾病找到了数千个疾病关联位点。在那时,GWAS就是基于芯片的CVAS研究的代名词。
但随着CVAS研究的进行,人们也渐渐认识到CVAS的局限。首先,常见突变并不能完全解释复杂疾病的遗传基础;更重要的是,CVAS定位的疾病关联位点大多分布于内含子区和基因间区,为确定基因型与疾病之间的功能性关系造成了很大的障碍。
基于测序的RVAS研究
低频突变关联分析(Rare variant association study, RVAS)是检测低频突变(MAF < 5% 或 MAF < 1%)与复杂疾病关系的方法。由于低频突变在人群当中频率较低,但基数极大;SNP分型芯片的设计基于已知突变,无法满足这类突变的检测需求,需要变异检测连续而全面的测序技术进行相关研究。
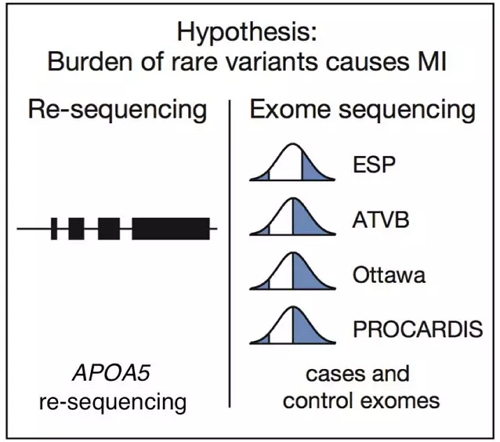
图2 心肌梗塞疾病的低频突变分析的设计方案
低频突变关联分析需要考虑以下几个方面:
1. 以连锁区域、基因、或通路为单位的关联分析:
RVAS与常见突变关联分析最大的不同在于rare variants频率较低,故RVAS不以位点为单位,而是以一段基因组区域为单位进行关联分析。常用方法包括SKAT, KBAC,CMC,WSS,Collapse等。
2. 突变的分布位置:
RVAS通常考虑编码区及Splicing区。因为非编码区突变的选择压力小,难以在适当样本量范围分析其统计学关联。
3. 突变类型的选择:
在RVAS分析中,可以采用多层次的关联分析不同类型突变与疾病的关系,包括:i) 非同义突变;ii) 有害性突变;iii) 功能丧失性突变;iv) 新生突变等。
4. 选样策略及关联策略:
基于特殊或较少研究的人种的RVAS分析有时可能产生令人兴奋的结果。同样,来自同一种族的对照在RVAS研究中也不能忽视。
寻找遗失的美好
传统的GWAS为我们提供了海量的信息,但也遗留下大量散落的拼图。而RVAS(低频突变关联分析)为我们理解复杂疾病的机理打开了一扇新的大门。高通量测序技术和日新月异的分析软件,让我们乘最快的马,奔最新的研究方向。
参考文献
Auer PL, Reiner AP, Leal SM.The effect of phenotypic outliers and non-normality on rare-variant association testing. Eur J Hum Genet. 2016 Jan 6. doi: 10.1038/ejhg.2015.270
Wu B, Pankow JS.Sequence Kernel Association Test of Multiple Continuous Phenotypes.Genet Epidemiol. 2016 Feb;40(2):91-100
Urrutia E, Lee S, Maity A, Zhao N, Shen J, Li Y, Wu MC.Rare variant testing across methods and thresholds using the multi-kernel sequence kernelassociation test (MK-SKAT).Stat Interface. 2015;8(4):495-505.
Mensah-Ablorh A, Lindstrom S, Haiman CA, Henderson BE, Marchand LL, Lee S, Stram DO, Eliassen AH, Price A, Kraft P.Meta-Analysis of Rare Variant Association Tests in Multiethnic Populations.Genet Epidemiol. 2016 Jan;40(1):57-65.
Wu B, Pankow JS, Guan W.Sequence Kernel Association Analysis of Rare Variant Set Based on the Marginal Regression Model for Binary Traits. Genet Epidemiol. 2015 Sep;39(6):399-405.
Moutsianas L, Agarwala V, Fuchsberger C, Flannick J, Rivas MA, Gaulton KJ, Albers PK; GoT2D Consortium, McVean G, Boehnke M, Altshuler D, McCarthy MI.The power of gene-based rare variant methods to detect disease-associated variation and test hypotheses about complex disease.PLoS Genet. 2015 Apr 23;11(4):e1005165.
Epstein MP, Duncan R, Ware EB, Jhun MA, Bielak LF, Zhao W, Smith JA, Peyser PA, Kardia SL, Satten GA.A statistical approach for rare-variant association testing in affected sibships. Am J Hum Genet. 2015 Apr 2;96(4):543-54.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
55
高大上
73
上档次
115
#GWAS#
41
?
80
蝴蝶效应,小的突变导致大的表观
83
技术发展太快,都是跟不上时代了
76