P Natl Acad Sci USA:百年验证,可行!溶瘤病毒登上“抗癌舞台”,是癌症免疫疗法
2017-08-06 佚名 生物探索
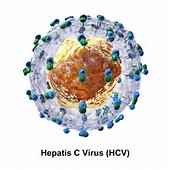
2006年,中国批准世界首个溶瘤病毒上市;2015年,安进肿瘤疫苗T-Vec成为美国FDA批准的首个溶瘤病毒疗法。经过一百多年的努力,溶瘤病毒这一“老概念”终于有了“新生命”。本专题回顾了这类“以毒攻毒”的疗法登上“抗癌舞台”的历程,同时分析了开发这类癌症免疫疗法所面临的独特挑战。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ACA#
33
#Nat#
30
#ATL#
33
谢谢分享,学习了
49
文章真好,赞赞赞
51
学习谢谢分享
60
联合治疗大势所趋。
42
学习
54