【一般情况】
男,45岁,汉族。
【主诉】
持续性胸痛1小时。
【病史摘要】
患者车祸后出现左侧胸部疼痛,呈压榨性,向左侧肩背部放散,含服硝酸甘油无明显缓解,就诊于笔者医院急诊,急查心电图(图6‐54‐1)诊断为急性心肌梗死。既往有高血压、高血脂病史。吸烟史20年,每日30支,无饮酒嗜好。
【查体】
患者神清语明,BP150/80mmHg。胸廓对称,双侧呼吸运动均等,叩诊清音,双肺呼吸音粗,双肺闻及散在干湿啰音。心前区无隆起,心界不扩大,心尖搏动位于第5肋间左侧锁骨中线内0.5cm,未触及震颤,心率78次/分,节律规整,各瓣膜听诊区未闻及杂音,无心包摩擦音。
【辅助检查】
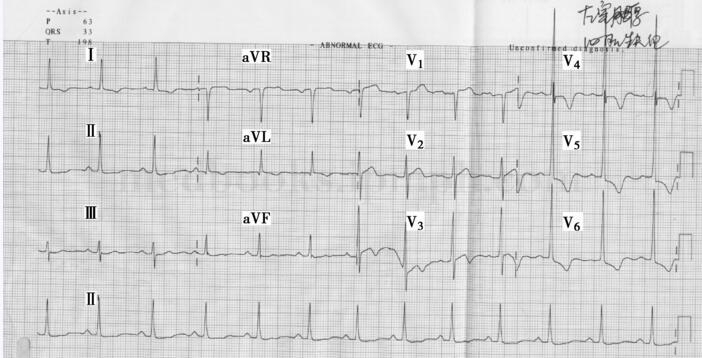
心电图检查见图6‐54‐1。急查心肌损伤标志物示肌钙蛋白0.04ng/ml,肌红蛋白403ng/ml,CK‐MB未见明显异常。再次复查心电图与入院时相比没有动态改变。
【初步诊断】
急性心肌梗死。
【病情分析】
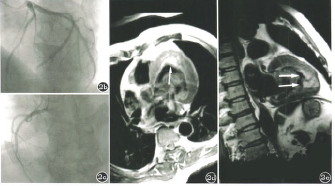
患者持续性胸痛,但心电图表现并不典型,且心肌损伤标志物无明显改变。考虑心电图改变有两种可能:①冠状动脉供血不足;②高血压所致左心室肥厚。如果想明确患者是否患心肌梗死,可以当即做冠状动脉造影。但是考虑患者胸痛的诱因是车祸,不能除外胸腔脏器外伤,所以没有急于进行冠状动脉造影,再次对患者进行详细查体,发现左侧胸部有压痛,嘱患者屏住呼吸,患者胸痛症状明显缓解。这时高度怀疑患者是外伤引起的胸痛,立即拍了床头胸片,并且请胸外科会诊,结果发现是左侧第7肋骨骨折,打上胸带以后患者症状明显缓解。症状发作12小时后复查肌钙蛋白为0.01ng/ml。病情稳定后为患者进行冠状动脉CTA,未见明显异常。综上所述,此患者胸痛是由于外伤造成的。该患者从症状上看酷似急性心肌缺血,心电图略有心肌梗死趋势,所以急诊医师考虑急性心肌梗死,从理论上说也是能理解的。但两次检测患者的心肌损伤标志物都在正常范围,而且心电图没有进行性改变,这两点不支持心肌梗死的诊断。如果盲目进行冠状动脉造影检查,会给患者带来不利。患者有外伤病史,若合并脏器内出血,给予阿司匹林、氯吡格雷会加重病情。
这个病例的体会是:
1﹒当遇到心前区疼痛,心电图有心肌缺血表现的患者时,需要详细询问病史及详细查体。尽管后来发现患者左侧胸部有压痛,但开始还是忽略了胸部的详细查体。心内科医师不能只注意心脏查体。
图6‐54‐1 心电图:窦性心律,V1~V3导联ST段略有抬高,V4~V6导联ST段下移,T波倒置
2﹒心肌损伤标志物对于诊断心肌梗死确实是非常重要的。此患者之所以没有考虑心肌梗死,主要是心肌损伤标志物没有动态变化,其心电图所示的心肌缺血考虑是左心室肥厚所致。cTnI/cTnT被美国和欧洲心脏病协会一致评为是诊断急性心肌梗死的高特异性和高敏感性的确诊标志物。在心肌细胞损伤早期,游离于胞浆内的cTnI/cTnT快速释放出来,血清/血浆中水平在4~6小时升高。随着肌原纤维不断崩解破坏,以固定形式存在的cTn不断释放,血清/血浆中cTn水平在AMI发生后8~14小时达高峰,1~2周后降至正常。由于cTnI/cTnT具有心肌特异性,胸痛发生4小时后的患者可直接检测cTnI/cT nT,其血清/血浆中水平升高具有诊断的特异性,AMI的早期诊断可为患者的治疗赢得宝贵时间。对于一直不能通过心电图改变诊断且无临床典型症状的微小心肌损伤患者,cTnI/cTnT的检测是目前的最佳辅助诊断指标。肌红蛋白是心肌损伤的最佳早期标志物。由于其为小分子物质,在急性心肌梗死(AMI)时可快速入血,故在AMI发生的1.5~6小时内,通过动态检测2次血清肌红蛋白水平可早期诊断是否有急性心肌梗死发生。如第2次检测值明显高于第1次,则具有极高的阳性预报价值;如动态检测2次测定值间无差异,则具有100%的阴性预报价值。
CK为细胞内重要的能量代谢酶,分布广泛,以肌细胞中最多,由2个亚基组成二聚体;CK‐MB主要存在于心肌细胞的外浆层,一直是临床诊断心肌损伤的心肌酶谱中最具特异性的酶,但长期以来用免疫抑制法测定酶活性的干扰因素很多,检测的敏感性、特异性均大受影响,目前仅推荐在无法测定肌钙蛋白的条件下应用。
对肌钙蛋白的升高应该结合临床表现,其升高除了见于急性心肌梗死,还见于心脏挫伤或其他外伤,包括外科手术、消融和起搏治疗等,急性和慢性充血性心力衰竭、主动脉夹层、主动脉瓣膜病、肥厚型心肌病、快速或缓慢型心律失常或心脏传导阻滞、心尖部气球样变综合征、心肌损伤导致横纹肌溶解、肺栓塞、严重的肺动脉高压、肾衰竭、急性神经系统疾病,包括脑卒中或蛛网膜下腔出血,浸润性疾病(如淀粉样变)、血色素沉着、结节病和硬皮病(如心肌炎或心内膜/心包炎累及心肌)、药物中毒或毒素、危重病,特别是伴有呼吸功能障碍或败血症,烧伤,尤其是影响到>30%的体表面积,过度劳累等情况。
其他非冠心病导致的急性心肌梗死,其他医院也有相关报道,如多发性大动脉炎、感染性心内膜炎均可能导致急性心肌梗死。
大动脉炎是一种全身性免疫系统疾病,临床累及冠状动脉并非少见,以女性为主,多累及冠状动脉开口。由于病变血管处理困难,通常要求待控制疾病活跃期后再进行手术治疗。在支架问世早期,即已有人开始将支架植入用于大动脉炎患者的冠状动脉,然而文献报告显示其再狭窄发生率很高,故不推荐用于此类患者。近年来,有个例报告,使用药物支架处理此类患者的冠状动脉狭窄获得较为理想的效果,笔者的经验也显示了类似获益。
多发性大动脉炎临床表现典型者诊断并不困难,但临床表现不典型者需要与其他病变鉴别。对年轻人,尤其是年轻女性,具有以下一种以上临床表现者,应怀疑或诊断本病:①单侧或双侧肢体出现缺血症状,伴有动脉搏动减弱或消失,血压降低或测不出;②脑动脉缺血症状,包括黑等TIA者,或伴有单侧或双侧颈动脉搏动减弱或消失者,或闻及颈部血管杂音;③近期发生的高血压或顽固性高血压,伴有上腹部Ⅱ级以上高调血管杂音;④无低热,血沉快,伴有血管杂音,四肢脉搏或血压有改变者;⑤病变累及肺动脉或冠状动脉,引起相应的临床症状者;⑥有多发性大动脉炎眼底改变者。另外,感染性心内膜炎发生急性心肌梗死的病例也有报道。据文献回顾表明,尸检显示感染性心内膜炎患者冠状动脉微栓塞发生率高达60%。冠状动脉栓塞的原因分为感染性和非感染性。常见病因包括二尖瓣和主动脉瓣瓣膜病、人工瓣膜、左心腔附壁血栓及冠状动脉介入。在二尖瓣前叶心内膜炎时,冠状动脉栓塞发生率高。链球菌、葡萄球菌及肠球菌感染是引起IE相关心肌梗死的主要细菌。少见病因包括肿瘤、反常栓塞、空气栓塞、钙化主动脉瓣上的碎片等。
冠状动脉栓塞患者的典型表现为易发生系统性栓塞疾病、猝死或胸痛,并伴急性心肌梗死特征性心电图和心肌酶变化。有时症状轻微,易被患者忽略,有时患者表现为气短加重或出现充血性心力衰竭,伴急性心肌梗死特征性心电图改变,但胸痛不典型或不伴胸痛,有时被误认为是瓣膜病或心内膜炎加重所致。70%的患者心电图改变为透壁性心肌梗死的永久性表现,30%表现为T波异常,并可恢复。对于老年、女性、合并高血压、首次侧壁或前壁MI、透壁性MI、无心绞痛史及左心室肥大患者,左心室游离壁破裂风险增加。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#标志物#
31
#心肌损伤#
42
#损伤#
37
好病历.学习了
56
学习了.有用
52