JAMA:对于非囊性纤维化支气管扩张患者 长期使用大环内酯类有利有弊
2013-03-30 高晓方 中国医学论坛报
澳大利亚与荷兰学者的两项研究(即BLESS和BAT研究)表明,在非囊性纤维化支气管扩张患者中,长期使用低剂量大环内酯类(红霉素和阿奇霉素)治疗可降低肺部感染加重发生率,但亦可升高大环内酯类耐药率。论文3月27日发表于《美国医学会杂志》[JAMA 2013,309(12):1251;1260]。 BLESS研究 共纳入117例在过去一年内出现2次及以上感染加重的非囊性纤维化
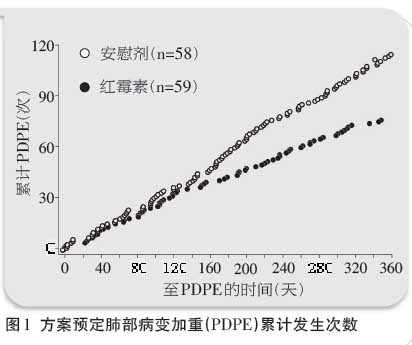
澳大利亚与荷兰学者的两项研究(即BLESS和BAT研究)表明,在非囊性纤维化支气管扩张患者中,长期使用低剂量大环内酯类(红霉素和阿奇霉素)治疗可降低肺部感染加重发生率,但亦可升高大环内酯类耐药率。论文3月27日发表于《美国医学会杂志》[JAMA 2013,309(12):1251;1260]。 BLESS研究 共纳入117例在过去一年内出现2次及以上感染加重的非囊性纤维化支气管扩张患者,并按照1:1比例随机给予为期12个月的琥乙红霉素(400 mg,2次/日)或安慰剂治疗。主要转归为方案预定肺部病变加重(PDPE)的年化平均发生率。 结果为,红霉素可显著降低总体PDPE发生次数[发病率比(IRR)为0.57,图1],并可在基线伴铜绿假单胞菌气道感染的预定亚组人群中降低PDPE发生率(P=0.02)。与安慰剂相比,红霉素可减少24小时咳痰量(P=0.01)并延缓肺功能减退(P=0.04)。红霉素可升高口咽链球菌的大环内酯类耐药率。 BAT研究 共纳入83例在过去一年出现3次及以上下呼吸道感染的非囊性纤维化支气管扩张患者,并随机给予为期12个月的
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#支气管#
43
#非囊性纤维化支气管扩张#
47
#长期使用#
36
#囊性#
36
#扩张#
51
#大环内酯类#
30
虽然能想象得到,但人家拿出结果
155