Prostate:前列腺癌早期检测新荧光探针研究
2019-08-10 AlexYang MedSci原创
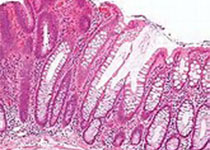
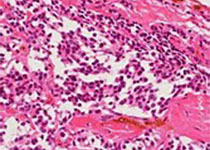
前列腺癌的早期检测能够明显的优化预后、延长患者寿命,并能够提高生活质量。已经有研究阐释了由于锌累积机制的损伤,前列腺癌组织具有比正常前列腺组织更低的锌含量。最近,有研究人员准备了一种新的基于吡咯并吡咯二酮(DPP)的荧光锌离子探针DPP-C2,且该新分子的荧光强度与环境锌离子的浓度成直接的比例关系。之后,研究人员在恶性肿瘤细胞(DU145和PC3细胞系)和正常前列腺RWPE-1细胞中进行了测试。研
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#探针#
30
#荧光#
28
#荧光探针#
41
#ROS#
24
#PRO#
32
前列腺癌相关研究,学习了,谢谢梅斯
46