NEJM:临床病例新栏目:lynch综合征相关的结直肠癌
2018-09-04 肿瘤资讯编辑部 肿瘤资讯
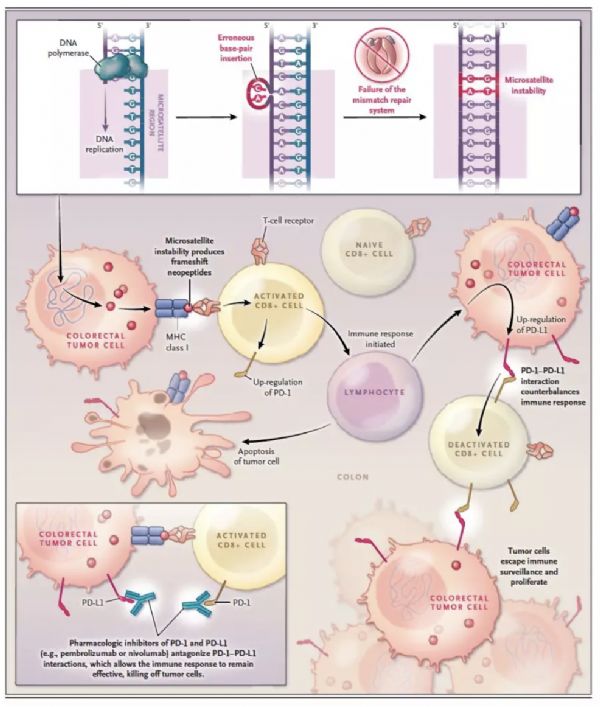
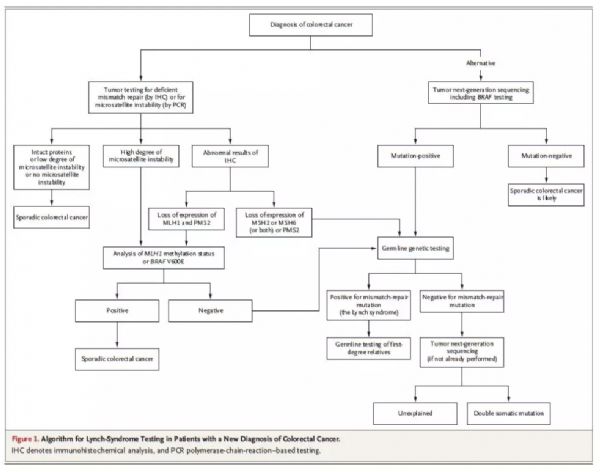
《新英格兰医学》杂志近期推出一个新栏目,以临床常见病例开头,然后呈现支持不同处理策略的证据,并回顾目前的治疗指南,最后以作者的临床推荐结束。最近一期NEJM杂志推出的病例为“Lynch综合征相关的结直肠癌”。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lynch综合征#
36
#综合征#
53
#结直肠#
32
好文章学习了!
85
好文章学习了!
59
好文章学习了!
79
好文章学习了!
74
好文章学习了!
67
很好的临床经验,值得借鉴!学习了,涨知识,受益匪浅,谢谢分享!
36