Front Neurol:椭圆形瞳孔研究现状
2019-03-25 不详 网络
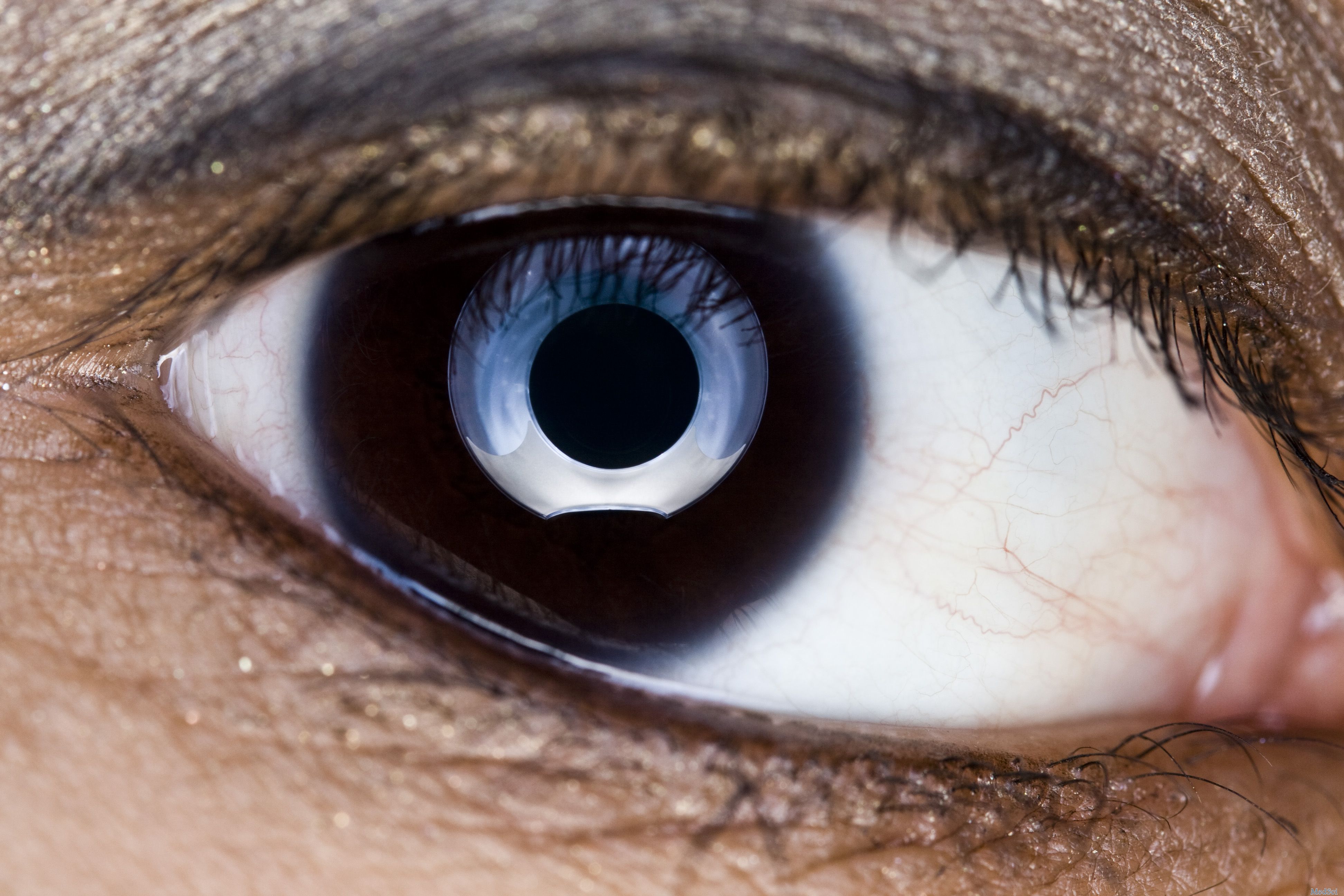
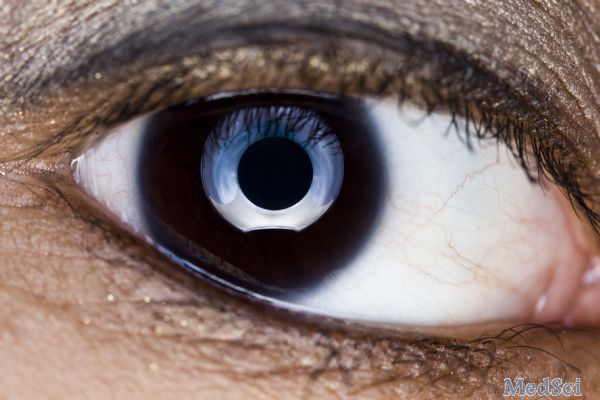
英国伦敦国立神经外科医院神经眼科的Bremner FD和美国新泽西州西海岸大学医学中心神经外科的Drapkin AJ两人近日在Front Neurol杂志上发表了一篇重要的综述文章,他们对卵圆形瞳孔的研究现状进行了分析,并阐述了它与瞳孔异位的区别以及它们在临床上的的不同意义。
英国伦敦国立神经外科医院神经眼科的Bremner FD和美国新泽西州西海岸大学医学中心神经外科的Drapkin AJ两人近日在Front Neurol杂志上发表了一篇重要的综述文章,他们对卵圆形瞳孔的研究现状进行了分析,并阐述了它与瞳孔异位的区别以及它们在临床上的的不同意义。
他们进行文献检索,发现有类似这种情况的实例只有20例临床病例。对这些病例的回顾研究,可以加深人们对此类疾病的认识,发现其致病性病变的最有可能的生理结构。作者也进行了深入讨论,对其致病的病理生理学机制进行了一些初步讨论。
原文出处:
Bremner, F.D. and A.J. Drapkin, The Dynamic Oval Pupil. Front Neurol, 2019. 10: p. 75.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#研究现状#
29
#椭圆形瞳孔#
21
#Neurol#
32
#瞳孔#
45
学习了
70
好
83