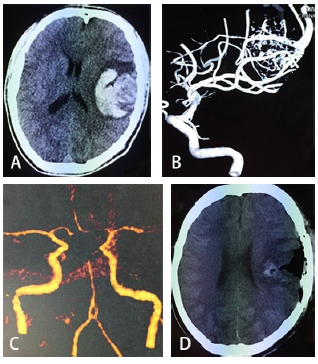
Neurology:脑动静脉畸形患者的长期健康相关生活质量
2019-09-12 xing.T MedSci原创
通过仔细选择患者,SPC B类患者可获得与SPC A类患者相同的HRQOL,提前是手术成功。应采取有效治疗以防止完全AVM闭塞,预防多次出血事件。AVM患者的术后治疗应侧重于预防抑郁症状、焦虑和癫痫发作。研究人员鼓励其他研究小组使用HRQOL工具充分了解神经病学和神经外科疾病对患者HRQOL的影响。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#动静脉畸形#
38
#静脉#
34
#Neurol#
26
#畸形#
33
#健康相关生活质量#
31